Introduction
Receiving a Parkinson’s disease diagnosis is a life-altering moment.
When that moment comes decades earlier than expected—sometime between the ages of 21 and 50—it brings a unique set of questions, challenges, and emotions.
A Young-Onset Parkinson’s Disease (YOPD) diagnosis forces a head-on collision with questions you never expected to ask so soon. It’s a profound interruption, challenging your identity, your plans, and your vision for the decades ahead.
But while the initial shock can feel isolating and overwhelming, it does not have to be defining. A diagnosis is not a conclusion; it is a turning point. It is the beginning of a journey where you learn to navigate, adapt, and take control.
This guide is for that journey. It’s not a story about limitations, but a roadmap for resilience, offering a proactive strategy to manage the disease and live a full, meaningful, and empowered life.
The Celeste (Light for PD) trial is showing promising results with a non-invasive approach to managing depression and other symptoms of Parkinson’s disease. Early findings suggest improved emotional well-being and quality of life for participants. Learn more about the study and how you can get involved.
What is Young-Onset Parkinson’s (YOPD) and How is it Different?
At its core, YOPD shares the same biology as its late-onset counterpart: the progressive loss of dopamine-producing cells in the brain.
Dopamine is a crucial chemical messenger that helps control movement, so this loss leads to the hallmark motor symptoms of Parkinson’s. However, the way the disease unfolds can be quite different.
One of the most significant differences is the rate of progression, which is typically much slower in YOPD.
People diagnosed at a younger age often remain independent and cognitively sharp for a longer period. But here lies a key paradox: because you live with the disease longer, you are exposed to medications for more years.
This leads to a higher and earlier likelihood of developing treatment-related complications like dyskinesia (involuntary movements) and motor fluctuations (“on-off” periods). This paradox shapes the entire treatment strategy from day one.

Here’s a quick comparison:
- Slower Progression: YOPD generally progresses more slowly, especially concerning cognitive decline and balance issues.
- Different Early Symptoms: YOPD often begins with dystonia (painful muscle cramping, like a foot turning inward) and rigidity, whereas late-onset PD more frequently starts with tremor and balance problems.
- Earlier Treatment Complications: People with YOPD tend to develop dyskinesias and “on-off” fluctuations sooner in response to the gold-standard medication, levodopa.
- Stronger Genetic Link: While most Parkinson’s is not directly inherited, genetics plays a much larger role in YOPD. A significant percentage of those diagnosed under 50, and especially under 30, have an identifiable genetic link.
Recognizing the Symptoms of Young-Onset Parkinson’s
Parkinson’s is widely perceived as a disease of the elderly, which is why the path to a YOPD diagnosis can be long and frustrating.
Many people spend years on a “diagnostic odyssey,” with early symptoms being misdiagnosed as sports injuries, carpal tunnel syndrome, a “frozen shoulder,” or simply stress. Understanding the wide range of symptoms is key.
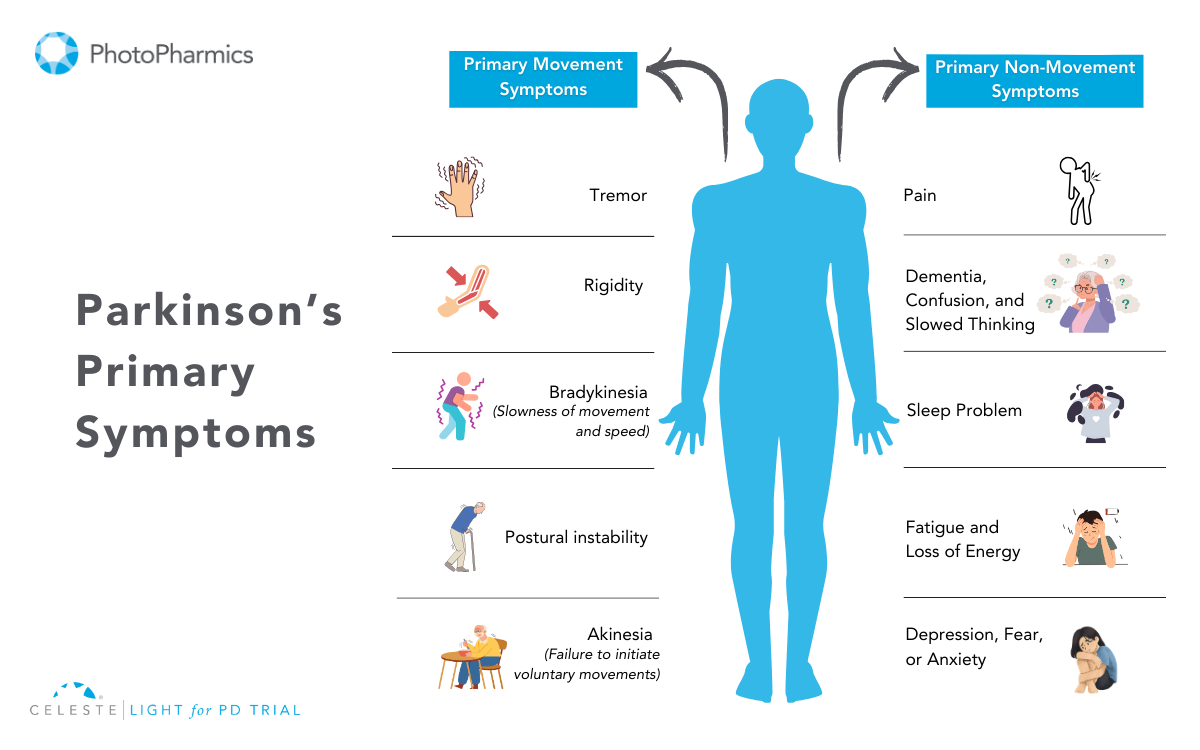
Motor Symptoms
While a resting tremor is a classic sign, it’s not always the first or most prominent one in YOPD. Look out for:
- Dystonia: As mentioned, this is a hallmark of YOPD. It can be a painful, sustained twisting or cramping in a limb, often a foot or hand.
- Rigidity: A stiffness in the arms, legs, or trunk that can be painful and limit your range of motion.
- Bradykinesia: This is a generalized slowness of movement that makes everyday tasks, like buttoning a shirt or writing, feel difficult and cumbersome.
- Tremor: Often starts in one hand at rest. In YOPD, it can sometimes be faster than the classic “pill-rolling” tremor.
The Invisible Burden: Non-Motor Symptoms
Often, the non-motor symptoms of YOPD can be more disruptive than the physical ones. They are a direct result of the same brain changes and are not just a reaction to the diagnosis.
- Depression and Anxiety: These are incredibly common and are considered an intrinsic part of the disease itself. They deserve to be treated as seriously as any motor symptom.
- Fatigue: A profound, debilitating sense of exhaustion that isn’t relieved by sleep.
- Sleep Problems: Insomnia and REM Sleep Behavior Disorder (physically acting out dreams) are frequent issues.
- Cognitive Changes: While severe dementia is rare in YOPD, you might notice more subtle difficulties with planning, multitasking, and problem-solving.
- Other common issues include loss of smell, constipation, and pain or tingling sensations.
The Genetic Puzzle of Young-Onset Parkinson’s
For many living with YOPD, the question “Why me?” quickly leads to “Is this genetic?”
The answer is complex, but the link is undeniable.
While the vast majority of Parkinson’s cases are idiopathic (meaning they have no known cause), a much larger percentage of YOPD cases are tied to specific genetic mutations. If you were diagnosed under 40, there’s a significant chance your condition has a genetic component.
Key genes associated with Parkinson’s include:
- PRKN (Parkin): Mutations in this gene are one of the most common causes of YOPD. It typically leads to a very slow-progressing form of the disease.
- PINK1 and DJ-1: Similar to PRKN, these genes are associated with early-onset, slow-progressing Parkinson’s.
- LRRK2 (Leucine-rich repeat kinase 2): This is the most common genetic contributor to late-onset Parkinson’s, but can also cause YOPD.
Genetic testing can provide clarity, help you understand potential risks for family members, and may qualify you for specific clinical trials targeting these genetic pathways. A conversation with a genetic counselor is the best first step to explore this option.
The Celeste (Light for PD) trial is showing promising results with a non-invasive approach to managing depression and other symptoms of Parkinson’s disease. Early findings suggest improved emotional well-being and quality of life for participants. Learn more about the study and how you can get involved.
Building Your Proactive YOPD Treatment Plan
Managing YOPD is a marathon, not a sprint. The goal is to balance effective symptom control now with preserving quality of life for the future. This requires a dynamic partnership with a multidisciplinary care team.
The “Levodopa Dilemma” and First-Line Therapies
Carbidopa/levodopa is the most powerful drug for PD symptoms. However, due to the high risk of developing motor complications, the strategy in YOPD is often to delay its use for as long as possible. To do this, doctors often start with other medications:
- Dopamine Agonists: These drugs mimic dopamine in the brain. They are effective but carry a significant risk of side effects, most notably Impulse Control Disorders (ICDs), such as compulsive gambling or shopping. This requires vigilant monitoring and open communication with your family and doctor.
- MAO-B Inhibitors: These medications provide a modest symptom benefit by helping the brain preserve its own dopamine. They are generally well-tolerated.
Eventually, levodopa will become necessary. At that point, the focus shifts to carefully managing doses and timing to keep you functioning well while minimizing side effects.
Advanced Therapies: A Strategic Move
For those whose motor fluctuations become difficult to manage with oral medications, advanced therapies are not a last resort but a proactive step to restore function.
- Deep Brain Stimulation (DBS): This surgical procedure acts like a “pacemaker for the brain,” using implanted electrodes to regulate the abnormal brain signals causing motor symptoms. For a person in their 40s or 50s, DBS can provide many years of improved function during peak career and family-raising years.
- Infusion Therapies: For severe fluctuations, continuous drug delivery via a small, wearable pump can provide a steady, reliable dose of medication throughout the day.
Lifestyle Management for Young-Onset Parkinson’s
Medical treatments are only one part of the equation. What you do every day can have a profound impact on your symptoms and overall well-being.
Exercise is Non-Negotiable
If there is one magic bullet in Parkinson’s care, it’s vigorous exercise. Research suggests it may even be neuroprotective, potentially slowing the disease’s progression. It helps your brain use dopamine more efficiently and builds new neural connections. Your goal should be to exercise with as much intensity as you can safely tolerate, as often as you can.
Build an “exercise cocktail” that includes:
- Aerobic Activity: Running, cycling, swimming, high-intensity interval training (HIIT).
- Strength Training: Using weights or resistance bands to combat muscle weakness.
- Mind-Body Practices: Non-contact boxing, dance (especially tango), Tai Chi, and yoga are fantastic for improving balance, agility, and coordination.
Nutrition for Brain Health
There’s no specific “Parkinson’s diet,” but a brain-healthy eating pattern can make a difference. The Mediterranean or MIND diets are highly recommended. They are rich in fruits, vegetables, whole grains, nuts, and healthy fats, which help fight inflammation and support cognitive function.
A crucial tip for those on levodopa: dietary protein can interfere with the medication’s absorption. Try taking your dose on an empty stomach (30-60 minutes before a meal) to maximize its effect.
Mental & Emotional Health: A Priority in YOPD Management
Depression and anxiety are not just reactions to a difficult diagnosis; they are clinical symptoms of Parkinson’s, caused by the same chemical changes in the brain that affect movement.
In YOPD, these non-motor symptoms can be particularly challenging, as you grapple with the disease’s impact on your career, finances, and family life. Prioritizing your mental health is as critical as managing your physical symptoms.
Strategies for emotional well-being include:
- Seek Professional Help: A therapist, counselor, or psychiatrist can provide invaluable tools for coping with the emotional toll of a chronic illness. Cognitive Behavioral Therapy (CBT) can be particularly effective.
- Consider Medication: Antidepressants can be very effective and should be discussed with your neurologist or a psychiatrist.
- Practice Mindfulness: Techniques like meditation and deep-breathing exercises can help manage anxiety and ground you in the present moment.
- Stay Connected: Resist the urge to withdraw. Lean on your support system and maintain social connections that bring you joy and a sense of belonging. Open communication with your loved ones is essential.
The Celeste (Light for PD) trial is showing promising results with a non-invasive approach to managing depression and other symptoms of Parkinson’s disease. Early findings suggest improved emotional well-being and quality of life for participants. Learn more about the study and how you can get involved.
Navigating Life, Work, and Relationships
A YOPD diagnosis forces you to re-evaluate everything. Open communication and proactive planning are your best tools.
Career and Disclosure
The decision to tell your employer is personal, but it’s a legal prerequisite for requesting workplace accommodations under laws like the Americans with Disabilities Act (ADA). Consider disclosing before your symptoms affect your performance, allowing you to control the narrative. Simple accommodations can make a world of difference:
- For tremor: Voice recognition software, ergonomic keyboards.
- For fatigue: A flexible schedule, options to work from home.
- For slowness: Modified deadlines, a self-paced workload.
- For concentration: Noise-canceling headphones in an open office.
Family and Parenting
Explaining YOPD to children can be daunting, but it’s essential. Use simple, age-appropriate language to explain symptoms, reassure them that it’s not their fault and not contagious, and maintain as much routine and stability as possible. The goal is to build trust and prevent them from inventing scarier explanations for what they see.
In a partnership, roles may shift, which can be stressful. Honest, vulnerable communication is the key to navigating these changes together. Redefine intimacy, focusing on emotional closeness and adapting your physical relationship as needed.
Finding Your Community, Looking to the Future
You are not alone. A vast network of support and a vibrant research community are working to make life better and find a cure.
- Connect with Others: Find a YOPD-specific support group, either locally or online. Sharing experiences with peers who truly understand is invaluable.
- Lean on National Foundations: Organizations like The Michael J. Fox Foundation, the Parkinson’s Foundation, and the American Parkinson’s Disease Association (APDA) are incredible resources for information, finding clinical trials, and connecting with local support.
- Stay Hopeful: The research landscape is more promising than ever, with advances in biological markers (like the alpha-synuclein seed amplification assay), precision medicine targeting specific genes, and therapies aimed at slowing the disease.
A diagnosis of Young-Onset Parkinson’s is the start of a new chapter, not the end of the book. By arming yourself with knowledge, embracing a proactive lifestyle, building a strong support team, and connecting with your community, you can navigate this journey with resilience, hope, and a continued sense of purpose.

A Bright Spot in Research: Our “Light for PD” Trial
For many living with Parkinson’s, the associated depression can be as debilitating as any motor symptom. We are pioneering a non-invasive, drug-free approach to managing this specific challenge. In recognition of its promise, our light therapy device has received a “Breakthrough Device” designation from the FDA for its potential to help manage PD.
Our current Phase 3 clinical study, the “Light for PD” trial, is investigating whether this specialized light therapy can improve the motor and non-motor symptoms of Parkinson’s. The trial has already shown a strong potential in managing depression associated with Parkinson’s.
Importantly, the trial is designed so that you can participate from the comfort of your own home, making it more accessible.
If you are interested in being part of the science that could change the future of Parkinson’s care, we encourage you to learn more about the “Light for PD” trial. You can discuss this opportunity with your neurologist or read all about it on our website to see if it might be a good fit for you.