Introduction
“My father experienced hallucinations and delusions, and at the time, we didn’t realize these symptoms were part of his Parkinson’s disease. My mom tried to shield my family and carry the burden alone each day. I wish l’d known there was more to Parkinson’s than motor symptoms, which is why l’m encouraging people and families affected by Parkinson’s to talk early and often about hallucinations and delusions.”
This heartfelt reflection by actor and advocate Ryan Reynolds highlights an often-overlooked reality: Parkinson’s disease is far more than tremors and motor issues.
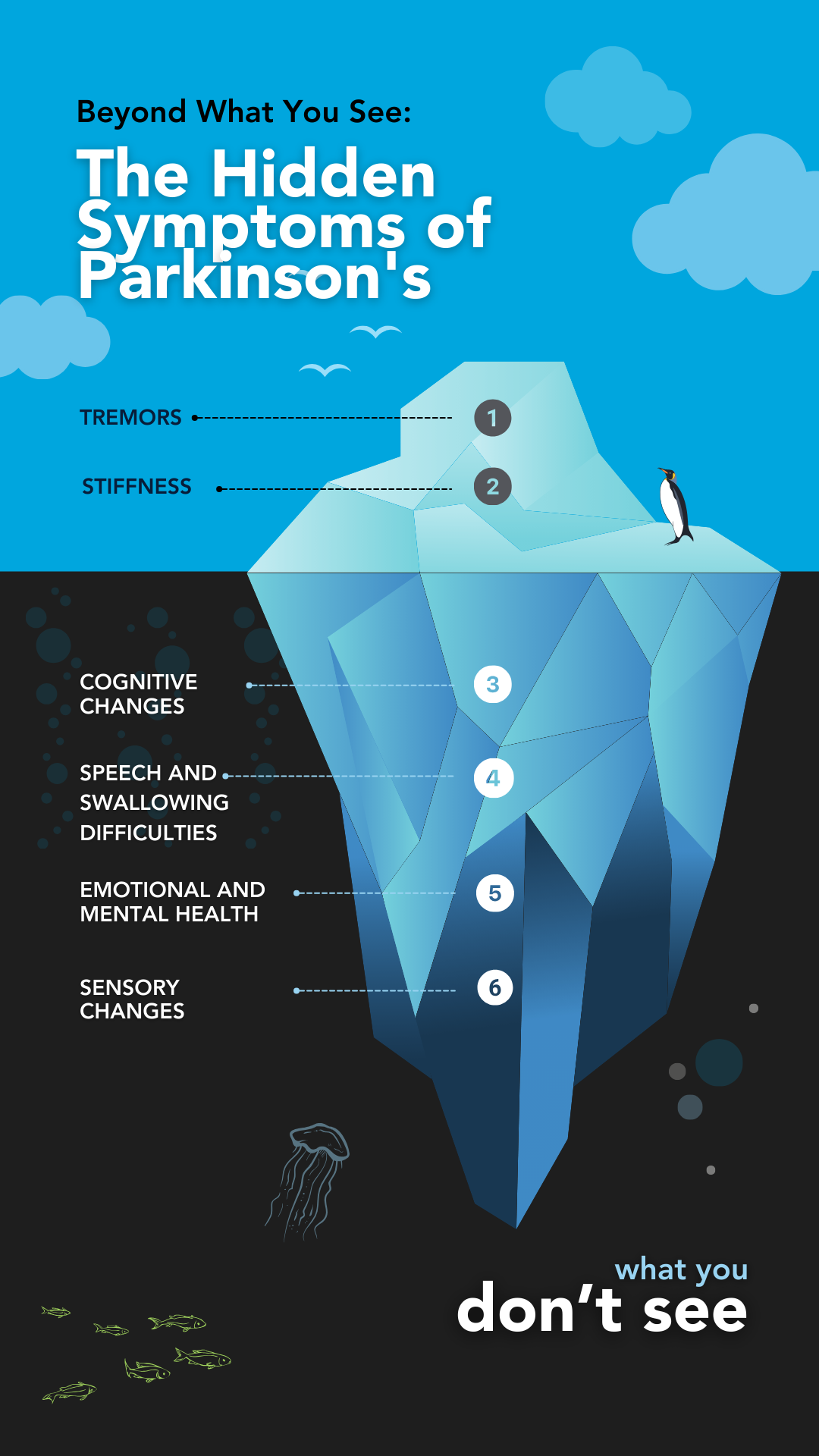
While most of us recognize Parkinson’s disease for its visible motor symptoms, these are merely “the tip of the PD iceberg.”
Beneath the surface lies a host of non-motor symptoms—such as hallucinations, delusions, sleep disturbances, anxiety, and cognitive changes—that can profoundly affect the quality of life for both patients and their caregivers.
In this article, we’ll dive deeper into the non-motor aspects of Parkinson’s disease, learn why they occur, and provide practical insights for managing these symptoms effectively.
Understanding the full picture of Parkinson’s is key to fostering better care, awareness, and support for those affected.
What are The Non-Motor Symptoms of Parkinson’s?
Parkinson’s disease (PD) is often recognized for its motor symptoms, such as tremors and stiffness. However, an equally significant aspect of PD is its non-motor symptoms, which can profoundly impact daily life.
These symptoms can precede motor signs by years, making early identification crucial.
Here’s a breakdown of the common non-motor symptoms, what they entail, why they occur, and their impact:
Cognitive and Emotional Challenges
- Cognitive Impairment: Issues like memory loss, slower thinking (bradyphrenia), and difficulty multitasking occur as Parkinson’s affects brain regions controlling cognition. Over time, this can progress to mild cognitive impairment or dementia.
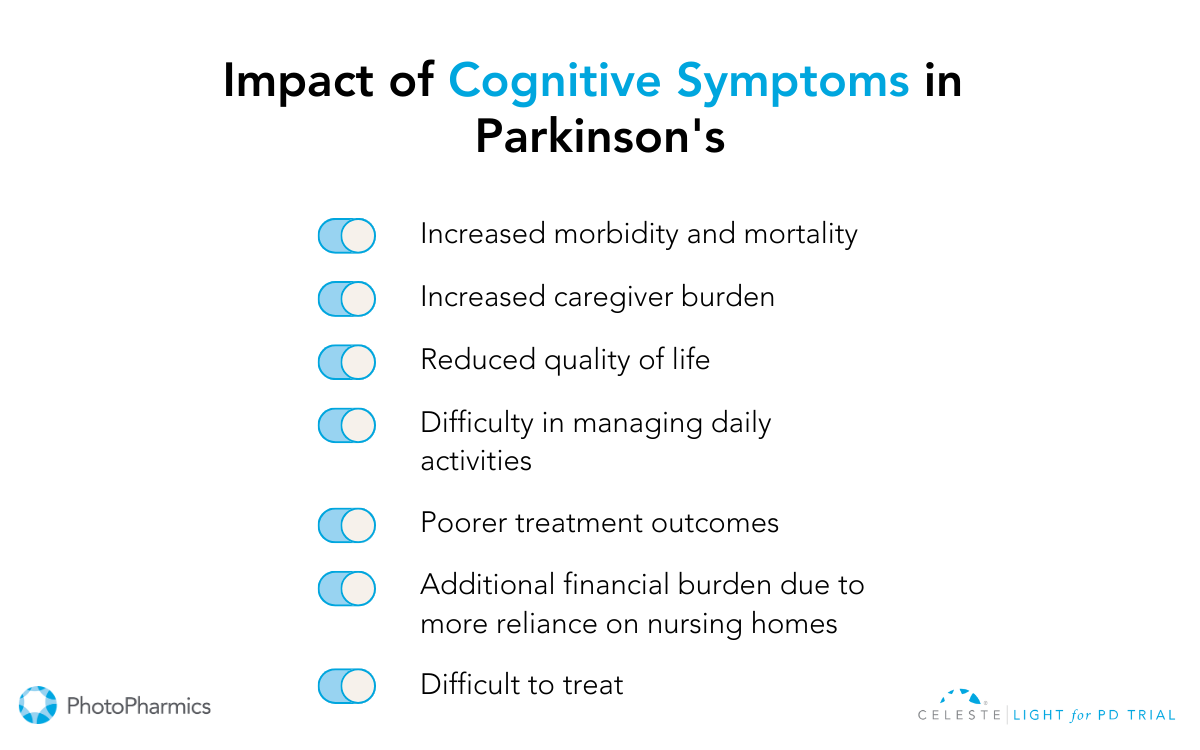
- Depression and Anxiety: Changes in brain chemistry, particularly dopamine levels, can trigger mood disorders. These conditions often begin early and can significantly affect quality of life.
- Hallucinations and Delusions: Hallucinations involve seeing or hearing things that aren’t there, while delusions are false beliefs. These symptoms are often associated with long-term use of Parkinson’s medications or disease progression.
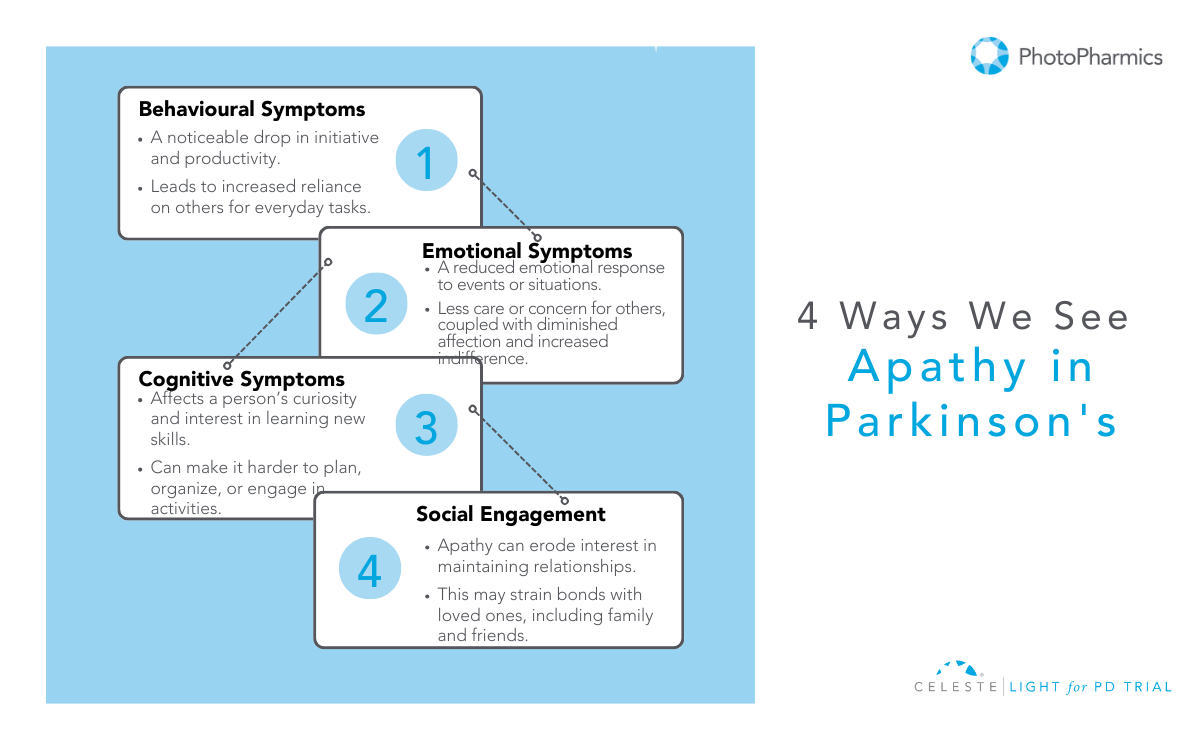
- Apathy: A lack of motivation that may be mistaken for intentional behavior but stems from neurological changes. It can significantly impact not only the person living with PD but also their loved ones. Apathy manifests in three ways:
— Cognitive: Reduced curiosity or interest in new things.
— Emotional: A lack of passion or reaction to events or news that would normally spark emotions.
— Behavioral: Difficulty starting activities and needing prompts to complete tasks.
Sensory and Autonomic Symptoms
- Skin and Sweating: Excessive sweating or oily skin is common due to overactive sweat glands. Dry skin can also occur in some individuals.
- Loss of Smell: Often one of the first signs of Parkinson’s, this is linked to early degeneration of specific brain cells.
- Pain and Tingling: Nerve dysfunction or rigidity can cause discomfort in various parts of the body.
- Rigidity: Stiffness throughout the body or in specific areas can lead to discomfort and restricted movement, often mistaken for normal aging.
- Autonomic Dysfunctions:
- Constipation: Impaired digestion due to slowed gut movement.
- Urinary Issues: A frequent need to urinate or incontinence caused by bladder muscle dysfunction.
- Lightheadedness: Sudden drops in blood pressure when standing (orthostatic hypotension).
- Sweating and Salivation: Overactive glands leading to excessive sweating or drooling.
Speech and Communication Issues
- Speech Problems: Many individuals experience reduced voice volume (hypophonia), monotone speech, or difficulty articulating words. This results from the reduced coordination of muscles involved in speaking.
Fatigue and Sleep Problems
- Chronic Fatigue: Often caused by disrupted sleep cycles, low dopamine levels, or medication side effects.
- Sleep Disturbances: These include difficulty falling asleep, vivid dreams, or REM sleep behavior disorder.
How To Manage Non-Motor Symptoms of Parkinson’s?
While it’s true that Parkinson’s disease currently has no cure, it doesn’t mean its progression cannot be delayed or its symptoms managed.
What does this mean?
Although you cannot eliminate Parkinson’s, you can slow down its progression and reduce its impact on your physical and mental health. This can be achieved by adopting certain lifestyle changes, such as maintaining a healthy diet, staying physically active, managing stress, and ensuring good sleep hygiene or taking targeted treatments.
Taking proactive steps can help you improve your quality of life and empower you to manage your condition better.

Cognitive and Emotional Challenges
Managing cognitive and emotional challenges in Parkinson’s Disease (PD) involves a multi-faceted approach that combines professional therapies and everyday strategies to enhance mental well-being and daily functionality.
Treatment Options and Tips:
-
Cognitive Remediation Therapy
This therapy focuses on teaching individuals alternative ways to manage memory or thinking problems by leveraging their cognitive strengths. It is particularly effective for those with mild cognitive deficits. Neuropsychologists or speech-language pathologists often conduct these sessions in a supportive environment, helping both individuals and caregivers apply practical strategies for daily tasks. While it doesn’t reverse cognitive challenges, it equips individuals with tools to improve their quality of life.
-
Behavioral Strategies
Simple environmental changes can reduce cognitive stress and confusion. Decluttering living spaces minimizes distractions while using nightlights can prevent disorientation during nighttime. Establishing a structured daily routine provides clarity and stability, which can help manage issues like impulsivity and difficulties with communication.
By incorporating these treatments and strategies, individuals with Parkinson’s and their caregivers can navigate cognitive and emotional hurdles more effectively, fostering a sense of control and improving overall quality of life.
Sensory and Autonomic Symptoms
- Sweating: Excessive sweating can be managed by adjusting carbidopa-levodopa doses under medical guidance. Lukewarm showers, lightweight clothing, and staying hydrated are practical tips to reduce discomfort, while severe cases may benefit from prescribed medications.
- Skin Issues: For dry or flaky skin, washing with warm water, using unscented glycerin soap, and applying moisturizers can help. Persistent issues like dandruff may require medicated shampoos or dermatological advice.
- Loss of Smell: No specific treatment is available, but monitoring dietary intake can help if appetite changes. Focus on balanced nutrition and seek guidance on maintaining a healthy weight if smell impacts eating habits.
- Pain and Tingling: To reduce stiffness, address nerve dysfunction through tailored exercises, such as stretching or yoga. Speak to your doctor about medications or therapies to effectively manage chronic pain. According to the Parkinson’s Foundation, some therapies used to manage the condition include Deep Brain stimulation (DBS), Botulinum Injections (Botox®), and surgery.
- Autonomic Dysfunctions:
- Constipation: To manage constipation effectively, incorporate a diet rich in fiber, including plenty of fruits, vegetables, and whole grains. Staying hydrated is equally important—aim to drink 48 to 64 ounces of water daily, and consider warm liquids in the morning to help stimulate digestion. Regular physical activity can further support healthy bowel function. If these measures aren’t sufficient, consult your doctor about adding fiber supplements or stool softeners to your routine.
- Urinary Issues: Monitor fluid intake to avoid overhydration while managing urgency. Discuss bladder training or medications with your doctor for better control.
- Lightheadedness: Stand up slowly to prevent sudden drops in blood pressure. Increase salt and water intake under medical supervision and wear compression stockings if advised by your doctor.
Speech and Swallowing Issues
Speech and swallowing challenges in Parkinson’s disease can be effectively managed through targeted therapies.
Managing Speech Issues
Speech-language pathologists (SLPs) play a critical role by tailoring exercises to improve vocal strength, clarity, and swallowing function. Evidence-based programs such as Lee Silverman Voice Treatment (LSVT) and Parkinson Voice Project SPEAK OUT! offer specialized support. For additional aid, assistive devices like voice amplifiers and exercises for articulation, posture, and breathing can enhance communication.
Further, maintaining hydration, practicing daily vocal exercises, and reducing background noise are key strategies to manage speech problems. Scheduling speech therapy early can help prevent worsening symptoms, and communication tools can support interactions.
Managing Swallowing Issues
Swallowing difficulties often benefit from dietary adjustments, such as softer food textures or thicker liquids, and exercises like expiratory muscle strength training, guided by an SLP.
Additionally, consulting an SLP for evaluation and following their recommendations, including modified diets and muscle training, ensures safer and more efficient eating to manage swallowing problems. Regular follow-ups and tailored interventions help improve quality of life.

Fatigue and Sleep Problems
Sleep challenges in Parkinson’s disease can often be managed with a combination of lifestyle changes, therapy, and medication.
- Maintaining a consistent sleep schedule, creating a calming bedtime routine, and ensuring a cool, dark sleeping environment can improve sleep quality.
- Daily outdoor activity and morning exercise help regulate the sleep-wake cycle, while light therapy can assist those unable to get outdoors.
- Limiting screen time and stimulating substances like caffeine before bed, as well as reducing fluid intake in the evening, can also minimize nighttime disruptions.
- For turning difficulties, satin sheets and pajamas or lightweight quilts are recommended.
Medical interventions can address specific issues like urinary frequency or medication side effects affecting sleep.
Doctors may prescribe medications such as oxybutynin or tolterodine for bladder-related disturbances (according to Parkinson’s Foundation), or antidepressants like mirtazapine for sleep support, though individual responses vary.
Consulting a sleep specialist or urologist for tailored treatments is advised. Avoiding anxiety-inducing activities and late-night heavy meals further supports restful sleep, ensuring better management of PD-related sleep concerns.
Be Part of the Light Against Parkinson’s: Participate in the Light for PD Clinical Trial
Managing Parkinson’s disease (PD) can be overwhelming, with many individuals experiencing persistent non-motor symptoms even after medications or surgeries.
PhotoPharmics is at the forefront of exploring innovative, non-invasive therapies to address these challenges. Our Light for PD clinical trial focuses on evaluating the Celeste therapeutic light device, designed to offer new hope for those living with PD.
This six-month, home-based study welcomes participants aged 45 and older with a Parkinson’s diagnosis and provides up to $500 for full participation.
By joining, you’ll contribute to groundbreaking research that could transform PD care while discovering a therapy with the potential to enhance your quality of life.
Check your eligibility today—let’s illuminate a brighter future together!