Introduction
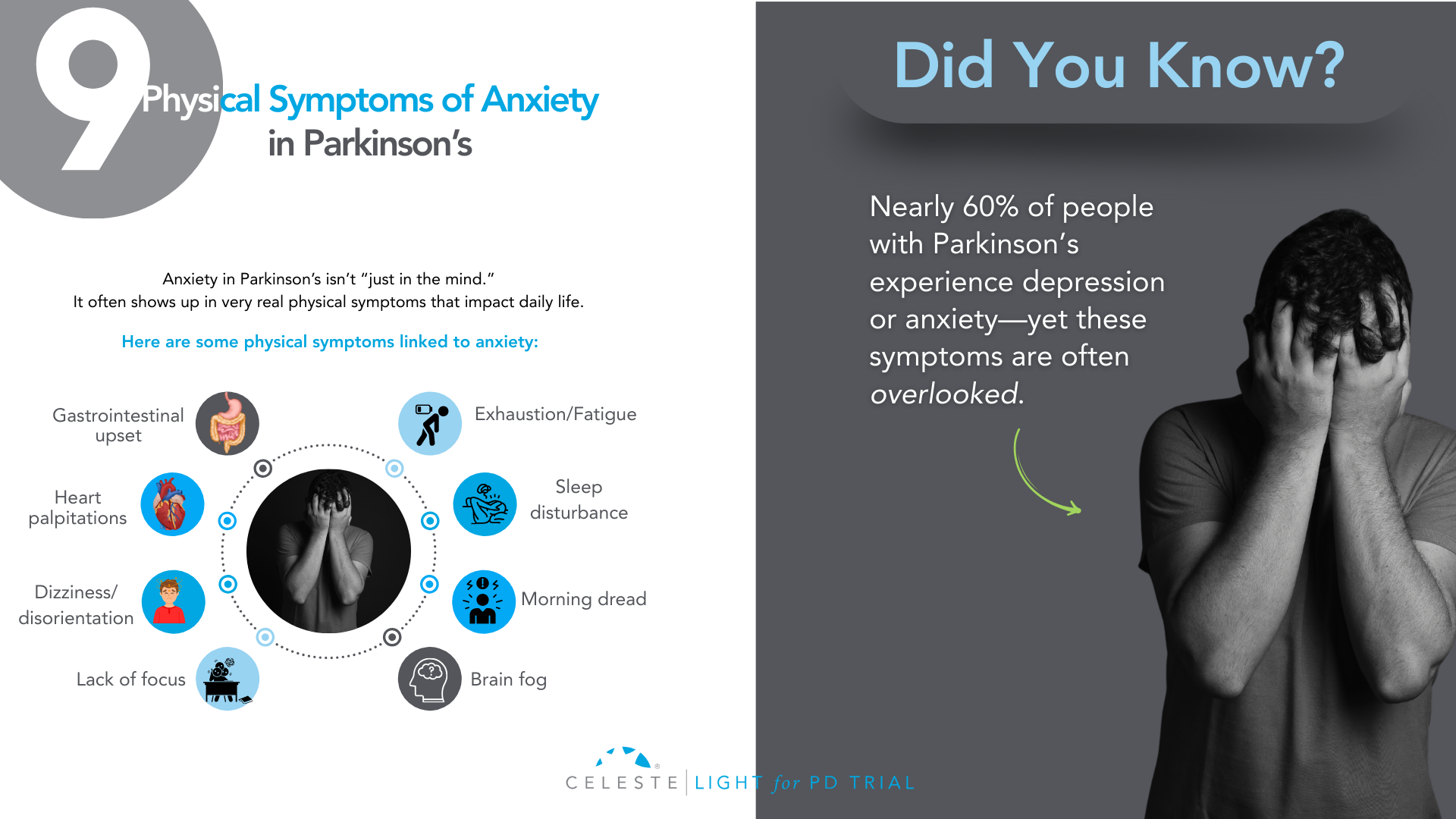
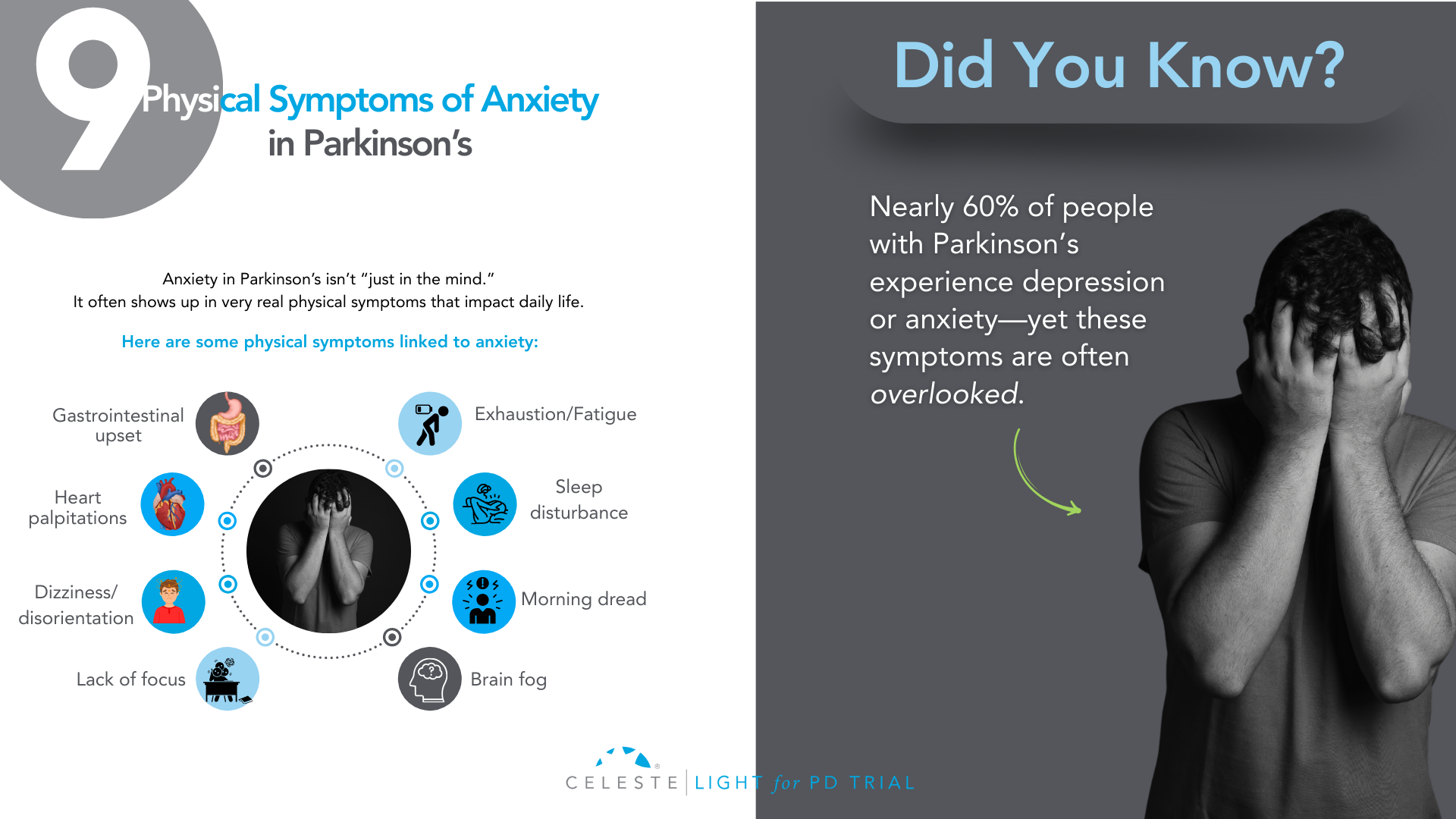
Did you know that at least 50% of people with Parkinson’s Disease (PD) will experience some form of depression during their illness, and up to 40% will face a significant anxiety disorder?
If you’ve been grappling with your mood, you are far from alone. For too long, the conversation around Parkinson’s has focused almost exclusively on the visible, motor symptoms like tremor, stiffness, and slowness.
But as you know, that’s only part of the story. The invisible challenges—the ones that happen inside—are often the heaviest to carry.
Many people, including doctors in the past, assumed that feeling down or anxious was just a natural emotional reaction to being diagnosed with a chronic illness.
While that can certainly be a factor, we now understand something much more profound: depression and anxiety are a core, biological part of the disease itself.
The same changes happening in your brain that affect movement are also affecting the chemistry of your mood.
This isn’t just a side issue; for many, it’s the main issue. It’s the hidden struggle that can impact your quality of life even more than the physical symptoms.
But here is the most important message: it is treatable. You do not have to “just live with it.”
This guide will walk you through this. We will explore why these feelings happen and look at what they look like in PD. This guide will discuss their impact on you and your loved ones. Most importantly, we will cover effective treatments. We will show strategies that can help you. You can reclaim your well-being.
The Celeste (Light for PD) trial shows promising results with a non-invasive approach to managing depression in Parkinson’s. Early findings point toward better support and improved quality of life. Find out how you can get involved.
Why Mood Changes Are Part of Parkinson’s?
To understand why mood changes are so common in Parkinson’s, we need to look beyond dopamine.
While PD is mainly caused by a loss of dopamine-producing cells, this is just one piece of a much bigger puzzle. The neurodegenerative process affects other crucial brain chemical systems as well. Think of it as a “neurotransmitter triad” involving dopamine, serotonin, and norepinephrine.
Role of Neurotransmitters
- Dopamine: This chemical is famous for its role in movement, but it’s also fundamental to our brain’s reward and motivation system. When the dopamine pathways that govern pleasure and drive are damaged, it can lead directly to apathy (a lack of motivation) and anhedonia (the inability to feel pleasure), which are core symptoms of depression.
- Serotonin: This is perhaps the most well-known mood-regulating chemical. The brain changes in PD also cause a significant loss of serotonin-producing neurons. This isn’t a side effect. It’s a direct hit on the system that helps keep our mood stable, our anxiety in check, and our sleep regulated. This direct link is a major reason why depression is so prevalent in PD.
- Norepinephrine: This chemical is essential for energy, focus, and our response to stress. The part of the brain that produces norepinephrine is also significantly affected in Parkinson’s. A drop in this chemical can contribute to the profound fatigue that so many experience, as well as to both depression and anxiety.
This complex, multi-system chemical imbalance explains so much. It tells us that what you’re feeling is real and has a physical cause. It also highlights one of the most compelling pieces of evidence: depression and anxiety often show up before any motor symptoms appear, sometimes by several years.
This strongly suggests that the mood-regulating parts of the brain are among the first to be affected by the disease process. Recognizing this can be empowering. It reframes your emotional struggles from a personal failing into a manageable symptom of your condition, just like a tremor or stiffness.

What Does Depression and Anxiety Look Like in Parkinson’s?
One of the biggest hurdles to getting help is that depression and anxiety don’t always look the way you’d expect, especially with Parkinson’s in the picture. There’s a significant and confusing overlap between the symptoms of PD and the symptoms of a mood disorder.
This clinical mimicry is a major reason why mood disorders are so often missed. You might feel fatigued and assume it’s “just the Parkinson’s.” Your family might see your reduced facial expression (hypomimia or “masked face”) and think you’re withdrawn or disinterested, when in reality it’s the PD affecting your facial muscles.
This is why it’s so critical to talk specifically about how you’re feeling on the inside, not just what’s showing on the outside.
Let’s break down how these conditions can manifest:
Depression in Parkinson’s can include:
- Major Depressive Disorder: This is what most people think of as clinical depression, involving a persistent low mood, loss of interest or pleasure, and other symptoms that make it hard to function.
- Minor Depression or Dysthymia: This is actually more common in PD. You may not meet the full criteria for major depression, but you experience a chronic, low-grade sadness and other depressive symptoms that still significantly impact your quality of life.
- Intense Feelings of Despair: We need to address this with care and honesty. For some, depression can lead to intense feelings of despair and even thoughts of not wanting to be alive anymore. If you ever find yourself having these thoughts, it is a medical emergency and a sign that the depression has become severe. Please understand that these thoughts are a symptom of the illness, and they can be treated. It is crucial that you reach out for help immediately—contact your doctor, a support hotline, or a trusted person in your life without delay.
The Celeste (Light for PD) trial shows promising results in addressing depression in Parkinson’s. This innovative research is exploring an innovative and non-invasive approach to improve your parkinson’s symptoms. Learn more and see if participation is right for you.

- Generalized Anxiety Disorder (GAD): This is a state of constant, excessive worry and nervousness that you can’t control. It can be accompanied by physical symptoms like a racing heart, sweating, or even a worsening of your tremor.
- Panic Attacks: These are sudden, intense episodes of overwhelming fear. In PD, they are often linked to medication “off” periods, when your motor symptoms return as your medication wears off. This can be terrifying, making you feel like you’re having a heart attack or can’t breathe.
- Social Phobia: This is an intense fear of being embarrassed or judged in social situations. It’s often driven by self-consciousness about visible symptoms like tremor, walking difficulties, or dyskinesias. This can lead to avoiding friends and family, causing profound isolation.
How Mood Impacts Your Life and Your Family?
If you’ve ever felt that your mood is a bigger problem than your tremor, you are not alone. Study after study has confirmed that for people with Parkinson’s, depression and anxiety are the single biggest factors that determine a person’s overall quality of life.
It’s not just about feeling sad; these mood states create a vicious cycle of disability that can touch every aspect of your life.
- Worsening Symptoms: Anxiety is known to make tremors worse. Both depression and anxiety are linked to more severe freezing of gait and the difficult “on-off” fluctuations.
- Undermining Self-Care: Depression saps the motivation you need to stick with your medication schedule, do your physical therapy exercises, and stay socially active—all things that are absolutely critical for managing Parkinson’s effectively.
- Accelerating Cognitive Decline: Mood and thinking are deeply connected. Untreated depression can make cognitive issues like problems with focus and attention worse, and over time, may even speed up the rate of cognitive decline.
This ripple effect extends far beyond the individual, placing an enormous strain on the family unit. For caregivers, managing a loved one’s psychiatric symptoms is often more distressing and exhausting than dealing with physical disabilities.
The caregiver’s well-being is directly tied to the patient’s mental state. It’s an incredibly stressful role, and studies show that a huge percentage of caregivers experience burnout and even clinical depression themselves.
Supporting the mental health of the person with Parkinson’s is one of the most important things we can do to support the health of the entire family.
Taking the First Step: Getting the Right Diagnosis
Given the challenge of symptom overlap, you have to be your own best advocate. Don’t wait for your doctor to ask about your mood. In the limited time of a neurology appointment focused on motor symptoms, it can easily be overlooked. You need to start the conversation.
Saying something as simple as, “I’d like to talk about how I’ve been feeling emotionally,” can open the door.
To help identify the problem, your doctor can use simple screening tools. These are short questionnaires that can quickly flag whether you need a more in-depth evaluation.
One of the most recommended for PD is the Geriatric Depression Scale (GDS-15). It’s useful because it focuses more on the psychological feelings of depression and asks fewer questions about physical symptoms that overlap with PD.
The goal of screening isn’t to give a final diagnosis, but to identify that there’s an issue that needs attention. The gold standard is always a full evaluation with a trained mental health professional, like a psychiatrist or neuropsychologist, who can fully understand the nuances of your situation and recommend the best course of action.

Building Your Treatment For Depression and Anxiety in Parkinson’s
Pharmacology is a key part of the treatment plan for many people. It’s about rebalancing the brain chemistry that the disease has disrupted. While no antidepressant is officially FDA-approved specifically for Parkinson’s, several types have been shown to be safe and effective.
Note: This information is for educational purposes only. We do not recommend self-treatment or medication. Please consult a healthcare professional for your Parkinson’s symptoms and receive personalized care options.
Available Options
- SSRIs (Selective Serotonin Reuptake Inhibitors): These are drugs like sertraline (Zoloft) or citalopram (Celexa). They are often the first choice because they are generally well-tolerated. They work by increasing the amount of available serotonin in the brain.
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): These are drugs like venlafaxine (Effexor) or duloxetine (Cymbalta). Because we know that both serotonin and norepinephrine are depleted in PD, these dual-action agents can be a very logical and effective choice.
- TCAs (Tricyclic Antidepressants): An older class of drugs, like nortriptyline, has some of the strongest evidence for effectiveness in PD. However, they come with more side effects (like confusion, dry mouth, and constipation) that can be especially problematic for older adults, so they are usually reserved for cases where other medications haven’t worked.
- Dopaminergic Medications: Sometimes, optimizing your Parkinson’s medication can itself have a positive effect on mood. Certain dopamine agonists (like pramipexole) have been shown to have antidepressant effects. And for anxiety or panic linked to “off” periods, adjusting the timing and dosage of your levodopa is often the most important intervention.
The key is working closely with your doctor. Finding the right medication and the right dose can be a process of trial and error, as suggested or followed by a healthcare specialist.
A thoughtful doctor will practice “symptom-focused prescribing,” choosing a medication that not only helps your mood but whose side-effect profile might help another symptom. For example, if you have depression and insomnia, a more sedating antidepressant might be a great choice.
Non-Medication Strategies For Depression and Anxiety in Parkinson’s
Medication is only one part of the solution. A truly comprehensive plan must include non-pharmacological approaches that empower you with skills and strategies to manage your mental health.
- Cognitive Behavioral Therapy (CBT): CBT is considered a first-line treatment for depression and anxiety in PD. It’s not just “talk therapy.” It is a practical, skills-based approach that teaches you how to identify, challenge, and change the negative thought patterns and behaviors that keep you stuck. For example, it helps you challenge thoughts like “I’m a burden to my family” and work on behavioral activation—scheduling small, achievable, and enjoyable activities to counteract withdrawal and apathy.
- Physical Exercise: Exercise might be a miracle drug for Parkinson’s. A huge body of evidence shows this. Regular activity is a powerful treatment. It’s effective for depression and anxiety. It boosts brain chemicals. It improves sleep. It gives you a sense of control. Find something you enjoy and do it consistently. This can be walking, Tai Chi, or yoga. It can also be a boxing class for PD.
- Social Connection: Isolation is fuel for depression. A lack of social support is one of the biggest risk factors for developing a mood disorder in PD. This is why support groups—either in person or online—can be a lifeline. Connecting with other people who truly “get it” reduces feelings of isolation and provides a space to share experiences and coping strategies.

You’re Not Alone—The Power of an Integrated Care Team in Parkinson’s Depression and Anxiety
Navigating Parkinson’s can feel like trying to coordinate a dozen different specialists who don’t talk to each other. The future of high-quality PD care is moving away from this fragmented system toward an integrated, multidisciplinary team model.
This means having a team of professionals who work together, with you and your family at the center. Your team might include:
- Your Movement Disorder Specialist, who manages the overall disease.
- A Psychiatrist or Psychologist, for medication management and therapy.
- A Clinical Social Worker, to help you connect with community resources.
- Physical, Occupational, and Speech Therapists, whose work to improve your function and independence has a huge positive impact on mood.
In this model, everyone is on the same page, working toward the same goal: improving your overall well-being.
Conclusion
Your emotional well-being is not a “soft” issue. It is not a secondary concern. It is central to your care. The depression and anxiety you feel are real. They are biological. They are treatable.
The first step is to acknowledge the struggle. Start a conversation with your doctor. Talk to your loved ones. Adopt a proactive and multimodal approach. Combine medications with other strategies.
Use therapy, exercise, and social connection. You can effectively manage your mood. Living with Parkinson’s is a journey. It has many challenges. But you don’t have to let this struggle define you. Bring it into the light. This is a crucial step. It helps you live well with Parkinson’s.
A New Ray of Hope: The LIGHT for PD Clinical Trial
For those looking for innovative, non-medication, non-invasive, and at-home approaches, there is promising research underway.
This study is the LIGHT for PD Trial, which is investigating the use of light therapy as a home-based treatment to potentially manage non-motor symptoms of Parkinson’s.
This approach is being explored as a safe, accessible way to potentially improve mood by helping to regulate the body’s internal clock. The trial especially shows promising potential in addressing depression in Parkinson’s.
However, it is close to its end with only 40 last sign-ups left.
So, if you are interested in exploring new treatment options and participating in important research, we encourage you to speak with your doctor or search online for the “LIGHT for PD Clinical Trial” to learn more about the study and see if you might be eligible to participate.
Introduction
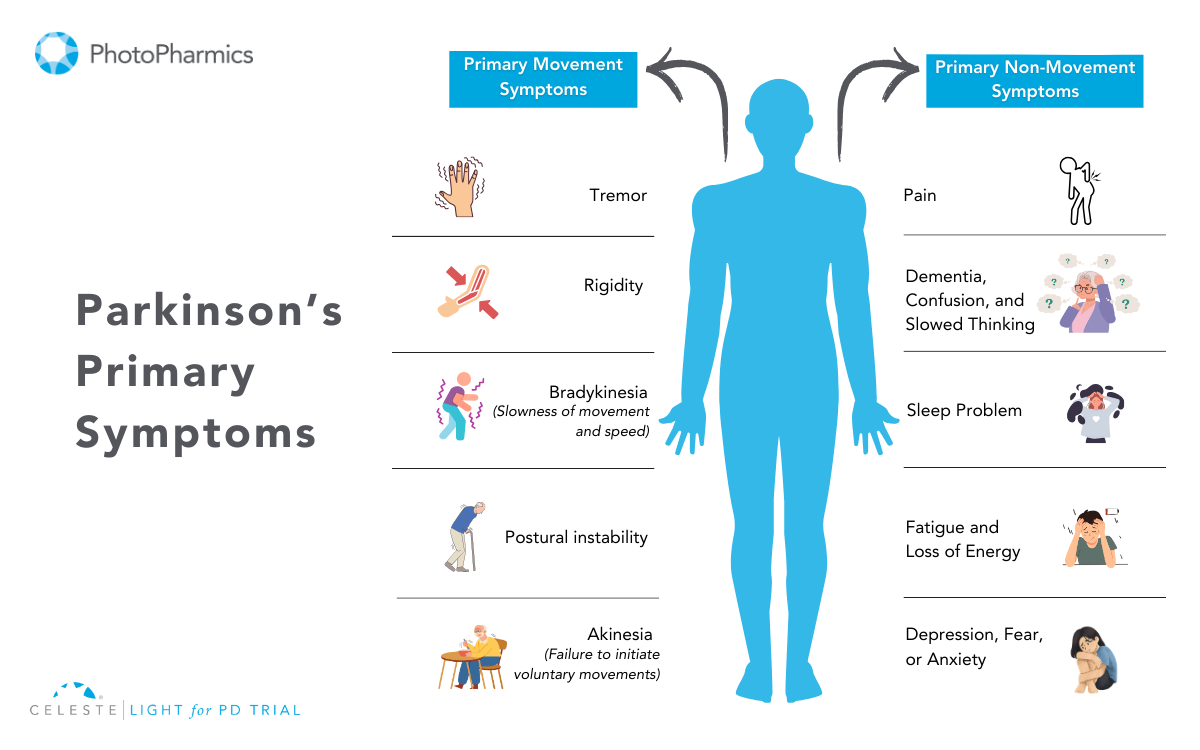
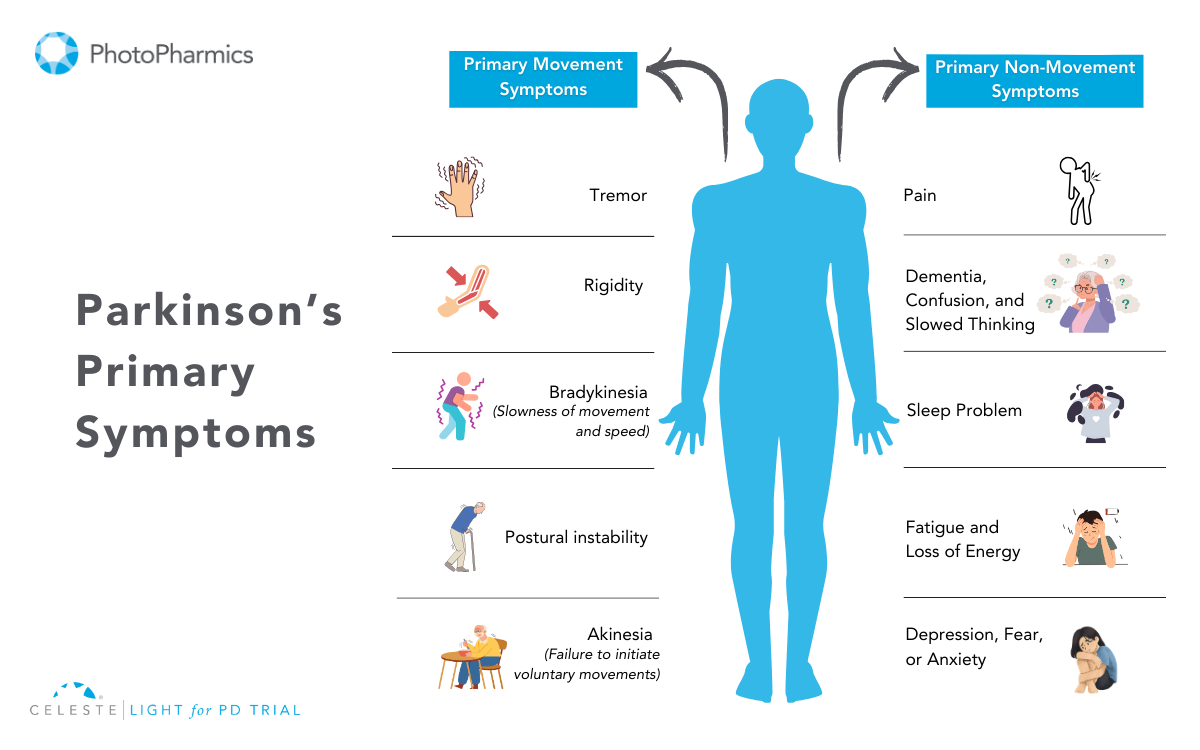
Parkinson’s Disease (PD) has long been associated with its cardinal motor symptoms: the tell-tale tremor, the stiffness that creeps in, the slowness of movement that makes everyday tasks a challenge, and the precarious dance of balance.
These are the signs that often lead to a diagnosis, the outward manifestations of a neurodegenerative process unfolding within the brain. However, the reality of Parkinson’s is far more nuanced, its onset is often heralded by subtle, seemingly unrelated changes that can precede the hallmark motor symptoms by months, years, or even decades.
Recognizing these early whispers, the subtle signs before the storm of motor impairment truly begins is becoming increasingly crucial for earlier detection, potential future interventions, and a more holistic understanding of this complex condition.
What Happens in Parkinson’s Before the Tremors?
For too long, the narrative around Parkinson’s has been dominated by its motor presentation. This focus, while understandable given the visible impact of these symptoms, has often overshadowed the significance of the non-motor changes that can act as early harbingers of the disease.
These subtle shifts in bodily function, sensory perception, and even mood can be easily dismissed as age-related quirks, the effects of stress, or indicators of other, more common ailments.
Yet, for a significant portion of individuals who will eventually be diagnosed with Parkinson’s, these seemingly innocuous changes are the first whispers of a neurodegenerative process already underway.
Understanding these early warning signs is not merely an academic exercise; it holds the potential to revolutionize our approach to Parkinson’s.
Earlier detection could pave the way for future neuroprotective therapies, and interventions aimed at slowing or even halting the disease’s progression before significant neuronal loss occurs.
Furthermore, recognizing these early symptoms can empower individuals to seek medical attention sooner, potentially leading to earlier symptom management and improved quality of life, even if disease-modifying treatments are not yet available.
So, what are these subtle clues, these whispers that might indicate the very early stages of Parkinson’s?
While the constellation of early symptoms can vary from person to person, several stand out as being more frequently reported and increasingly recognized as potential prodromal markers of the disease:
The earliest changes occur when the brain’s dopamine-producing neurons—critical for controlling movement—begin to deteriorate silently.
But Parkinson’s also impacts parts of the nervous system that regulate sleep, smell, digestion, mood, and cognition.
This means that many of the first signs of PD show up outside of movement. These are called non-motor symptoms, and understanding them can offer the first clue that something deeper is happening.

Early Non-Motor Symptoms to Watch For Parkinson’s
1. Loss of Sense of Smell (Hyposmia)
One of the most consistently reported and well-researched early non-motor symptoms of Parkinson’s is a diminished or complete loss of the sense of smell, a condition known as anosmia.
Often dismissed as a consequence of a common cold or allergies, a persistent and unexplained decline in the ability to detect odors can be a significant early indicator.
The olfactory bulbs, the brain regions responsible for processing smell, are among the first areas affected by the accumulation of alpha-synuclein, the protein hallmark of Parkinson’s. Studies have shown that a significant percentage of individuals newly diagnosed with PD report experiencing a loss of smell, often years before the onset of motor symptoms.
While not everyone with anosmia will develop Parkinson’s, its presence, especially when accompanied by other subtle changes, warrants attention.
2. Constipation
Changes in bowel habits, particularly the development of chronic constipation, are another frequently reported early symptom of Parkinson’s. The enteric nervous system, the network of nerves in the gut, is also affected by the accumulation of alpha-synuclein.
This can lead to a slowing of gut motility and subsequent constipation, often occurring years before motor symptoms manifest. While constipation is a common ailment with various causes, its persistent and unexplained onset, particularly in younger individuals without other obvious contributing factors, should raise a degree of suspicion.
Some experts believe that Parkinson’s may even start in the gut and migrate to the brain.
3. Sleep Disturbances (Especially REM Sleep Behavior Disorder)
REM Sleep Behavior Disorder (RBD) is a fascinating and often vivid early warning sign. During the Rapid Eye Movement (REM) sleep stage, our bodies are typically paralyzed, preventing us from acting out our dreams.
In RBD, this paralysis is absent, leading individuals to physically act out their dreams, sometimes violently, potentially causing injury to themselves or their bed partners. Vivid dreams, talking or yelling during sleep, and even physically acting out dreams are strong predictors of Parkinson’s later in life.
RBD is strongly linked to an increased risk of developing synucleinopathies, including Parkinson’s and Lewy body dementia. A significant proportion of individuals with RBD will eventually go on to develop one of these conditions, often years after the onset of RBD

4. Depression and Anxiety
Subtle shifts in mood, particularly the emergence of depression and anxiety, can also precede the motor symptoms of Parkinson’s. These mood changes are not simply a reaction to the eventual diagnosis but are believed to be a direct consequence of the neurochemical changes occurring in the brain.
Alterations in dopamine, serotonin, and other neurotransmitter systems, even in the early stages of the disease, can contribute to feelings of sadness, apathy, and heightened anxiety.
While mood disorders are common, their new onset or a significant change in their pattern, especially when accompanied by other potential early signs, should be considered within the broader clinical picture.
Depression isn’t just a reaction to Parkinson’s—it can actually precede diagnosis.
5. Fatigue
Persistent exhaustion that doesn’t improve with rest is another early non-motor symptom. Fatigue can feel overwhelming and may occur well before diagnosis, impacting daily life and energy levels. It can make even simple activities feel disproportionately difficult, affecting work performance, social engagement, and motivation.
Unlike ordinary tiredness, Parkinson ’s-related fatigue often doesn’t resolve with sleep, making it a persistent and frustrating challenge for many.

Early Motor Symptoms: The First Physical Signs of Parkinson’s
While non-motor symptoms often appear first, early motor changes are still critical clues.
1. Smaller Handwriting (Micrographia)
People may notice their handwriting becoming small and cramped, a condition known as micrographia. This subtle change, often appearing gradually, is one of the earliest motor symptoms and can occur even before noticeable tremors manifest.
It can start with just a few words shrinking on a page and may progress over time. Paying attention to such fine motor skill changes can be an important clue for early detection.
2. Slowness of Movement (Bradykinesia)
Everyday tasks—like buttoning a shirt or walking—become noticeably slower and require more conscious effort than before. This slowness of movement, known as bradykinesia, is a hallmark of Parkinson’s and is often one of the first movement-related symptoms to emerge.
It can manifest as a general feeling of sluggishness or difficulty initiating movements. Over time, bradykinesia can impact a wide range of activities, making routine tasks increasingly challenging.
3. Subtle Changes in Walking or Posture
A slight shuffle in their walk, a noticeable decrease in the natural swing of their arms while walking, or the development of a subtly hunched posture may appear early on. These changes in gait and posture can be gradual and easily overlooked initially.
Often, family members, close friends, or observant colleagues notice these subtle physical alterations before the individual experiencing them becomes consciously aware. Bringing these observations to the attention of a healthcare professional can be a valuable step in the early identification process.

4. Facial Masking
Reduced facial expression—sometimes called “facial masking” or hypomimia—can cause people with early Parkinson’s to look serious, sad, or even depressed even when they feel perfectly fine internally. This flattening of affect is a subtle but noticeable change in how emotions are outwardly conveyed.
It’s a direct result of the reduced automatic muscle movement in the face, making it harder to display a full range of expressions spontaneously. Your loved ones might comment that the person seems less animated or expressive, even in joyful situations.
5. Softer Voice
Subtle alterations in speech patterns, such as a softer voice (hypophonia) or a more monotone delivery, can also be early indicators. These changes, often not readily apparent to the individuals themselves, might be noticed by close family members or friends.
They are thought to be related to early changes in the motor control of the vocal cords and respiratory muscles.
(Source: Parkinson’s Foundation)
Why Recognizing Early Symptoms of Parkinson’s Matters?
The significance of recognizing subtle early warning signs of Parkinson’s cannot be overstated. While having one or even several of these symptoms does not definitively mean someone will develop Parkinson’s, their co-occurrence and persistence—especially without other clear causes—should prompt consultation with a neurologist.
Why does early recognition matter?
- Subtle symptoms can precede obvious motor issues by years.
- Co-occurring non-motor changes often hint at underlying neurological shifts.
- Seeking timely evaluation may lead to better monitoring and management.
Increased awareness among the general public and healthcare professionals is crucial. Educating individuals about the significance of these minor changes can empower them to seek medical advice early. For clinicians, understanding these early signs can mean faster referral to specialists and the chance to initiate monitoring strategies sooner.

What Should You Do If You Notice Early Symptoms?
If you or someone you know shows a combination of these symptoms:
- Make an appointment with a neurologist—preferably one specializing in movement disorders.
- Keep a written log of symptoms to share with your doctor.
- Ask about seeing a physical therapist, occupational therapist, or speech therapist even before diagnosis to maintain function and confidence.
- Stay active and pursue an exercise program tailored for brain health. Seek emotional support—both counseling and peer groups can make a difference.
(Source: Parkinson’s Foundation)
Conclusion: Don’t Wait for the Tremor
Parkinson’s disease is often thought of as a “movement disorder.” But the truth is, the journey starts quietly—long before the first visible tremor.
If we start recognizing the early warning signs, we can push toward earlier diagnoses, better treatment plans, and improved outcomes for those affected.
Awareness is power. Trust your instincts. Seek answers early.
And always remember: Parkinson’s does not define a person—early action empowers them.
Interested In New Ways To Manage Parkinson’s Non-Motor Symptoms?
Beyond the motor challenges of Parkinson’s, non-motor symptoms such as sleep disturbances, mood disorders, and fatigue can significantly impact quality of life. As research advances in diagnosing Parkinson’s, innovative approaches are also emerging to help manage the condition’s impact.
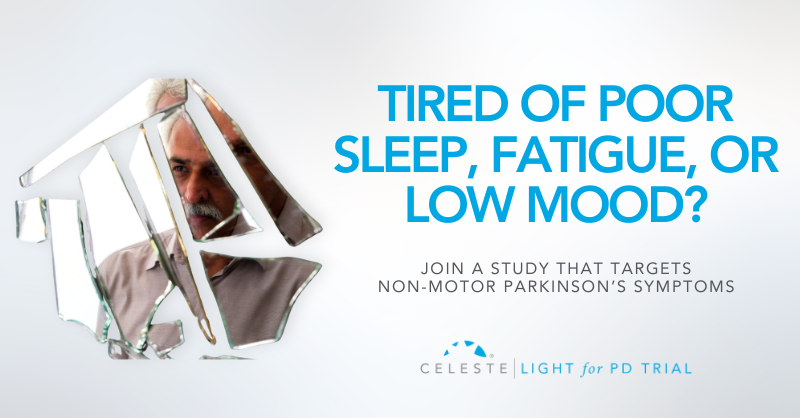
For instance, Light for PD (our ongoing Parkinson’s clinical trial) is exploring the benefits of light therapy for managing non-motor symptoms of Parkinson’s.
This non-invasive, at-home therapy offers a promising option to improve the quality of life for those living with PD. By targeting symptoms such as sleep disturbances and mood changes, Light for PD provides a gentle, science-backed way to complement existing treatment plans.
If you or someone you know is navigating Parkinson’s, consider joining this trial to explore a new pathway to relief.
For more information to check your eligibility, visit www.lightforpd.com.
Introduction
Parkinson’s is one of the most common neurodegenerative disorders, second only to Alzheimer’s. Globally, it affects around 1% of people over 60, making it the leading movement-related neurological condition.
“Parkinson’s diagnosis and treatment options” is one of the most common concerns for individuals living with Parkinson’s and their families. The uncertainty surrounding symptoms, medical evaluations, and treatment plans can feel overwhelming.
That’s why we’ve created this guide—to answer your most pressing questions and help you navigate the path forward with clarity and confidence.
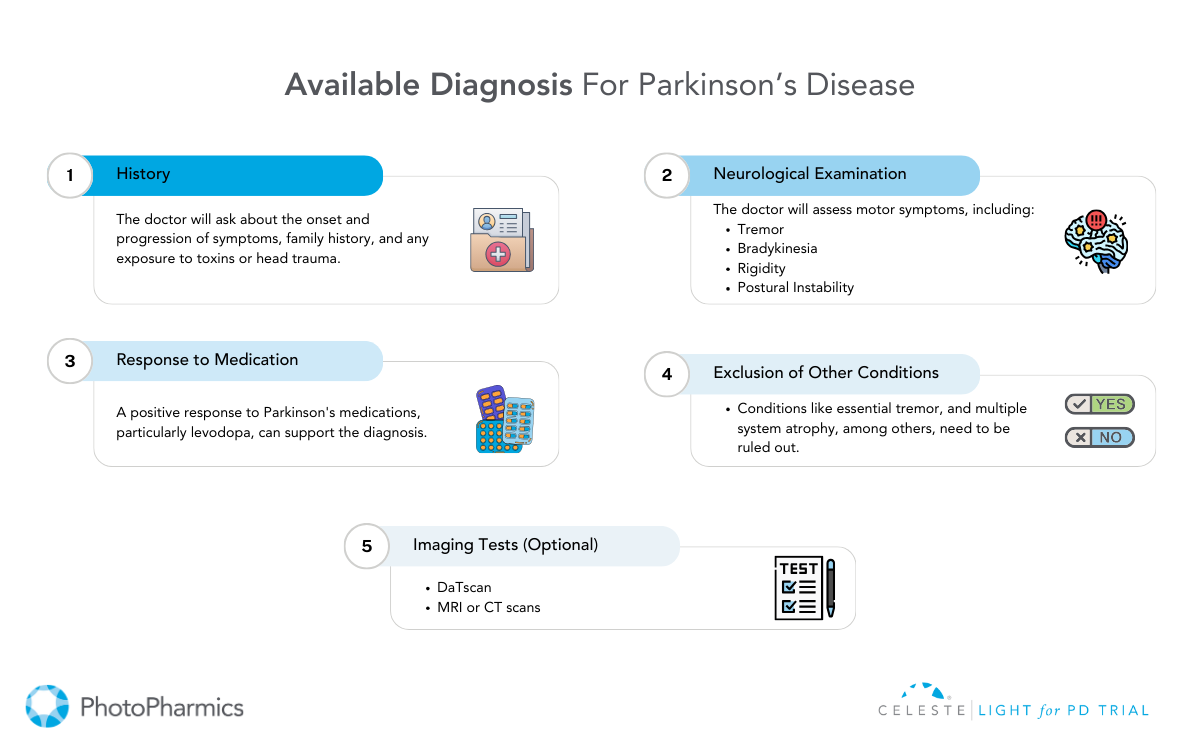
Parkinson’s disease is a progressive neurological condition that affects movement, coordination, and other vital functions. Because symptoms often develop gradually, diagnosing Parkinson’s can be complex, requiring a detailed medical history, neurological exams, and, in some cases, advanced imaging tests.
While there is no single definitive test, early and accurate diagnosis is key to managing the condition effectively.
Once diagnosed, treatment options vary depending on the stage of the disease and individual needs.
From medications that help manage symptoms to therapies like physical and occupational therapy, each approach aims to enhance quality of life. In more advanced cases, surgical interventions such as deep brain stimulation (DBS) may offer relief. Additionally, emerging treatments and clinical trials provide hope for future breakthroughs.
While Parkinson’s presents challenges, proactive management, and the right treatment plan can make a significant difference. I
In this article, we’ll explore the available diagnostic tools, current treatments, and promising advancements in Parkinson’s care, helping you or your loved one take informed steps toward better health and well-being.

1. Understanding Parkinson’s Disease
Parkinson’s disease is a disorder that gradually affects the brain’s ability to control movement. It occurs due to the deterioration of nerve cells in a region called the basal ganglia, which leads to a decline in dopamine production. Dopamine is essential for smooth and coordinated muscle activity, and its deficiency causes symptoms like tremors, muscle stiffness, and slowed movement.
However, Parkinson’s isn’t just a movement disorder. As it progresses, it can affect various aspects of life, including cognition, mood, sleep, and sensory functions. Many individuals experience depression, memory challenges, and difficulties with speech or swallowing. Though no cure exists, early diagnosis and proper management can significantly improve daily functioning.
Who is at Risk?
Parkinson’s is primarily an age-related condition, with most cases diagnosed around 60 years old or older. The risk increases with age, but it is not limited to the elderly. A small percentage of cases, known as early-onset Parkinson’s, occur in younger adults, sometimes as early as their 20s or 30s. These cases are often linked to genetic factors, meaning a close relative may also have had the disease.
Men are slightly more likely than women to develop Parkinson’s, but the reason behind this difference remains unclear. Scientists continue to study genetic and environmental factors that may contribute to disease onset.
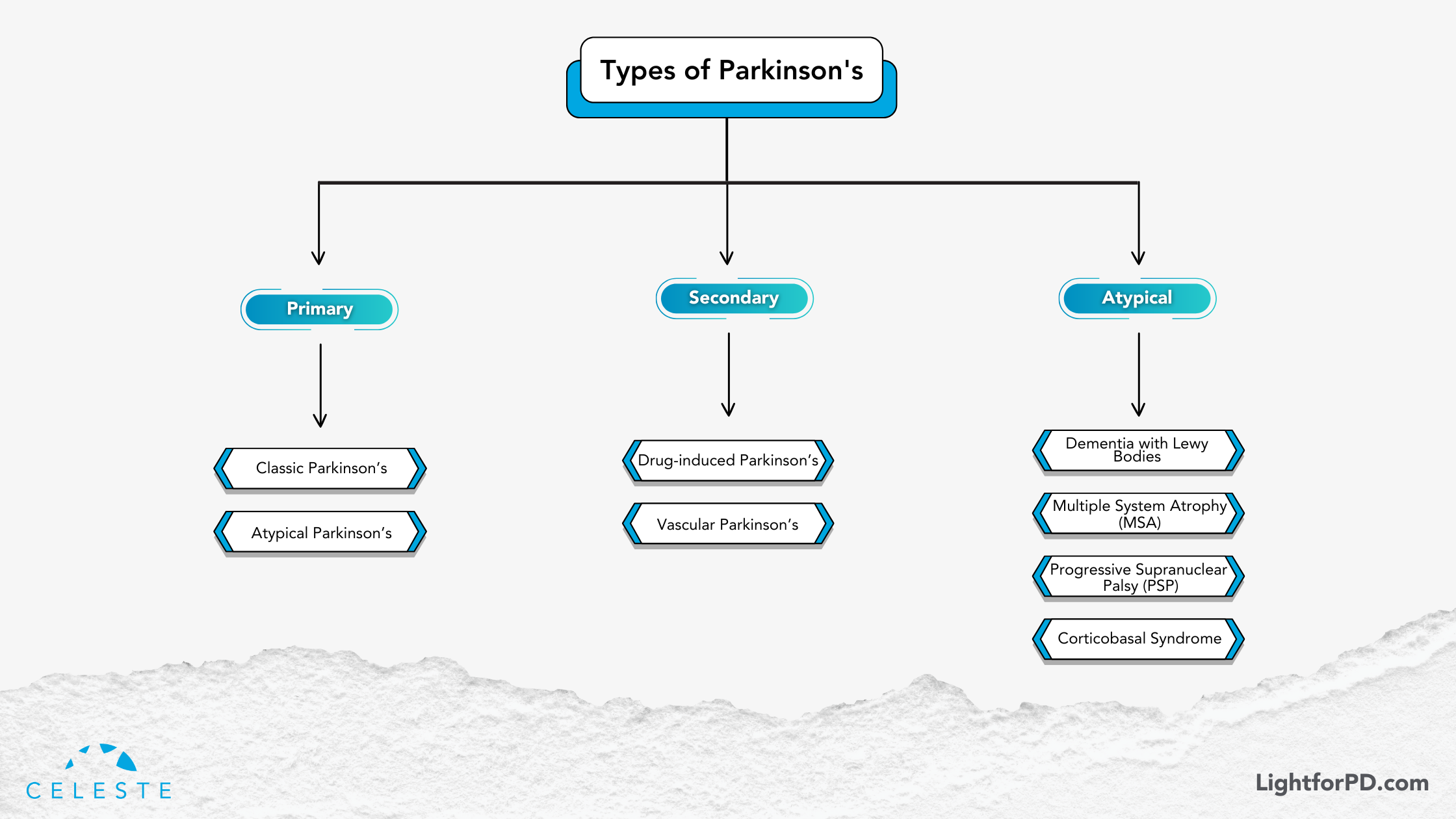
Parkinson’s and Related Conditions
The term “parkinsonism” is a broader term that includes Parkinson’s disease and other conditions that have similar symptoms. These other conditions might include multiple system atrophy or corticobasal degeneration.
Parkinson’s disease, specifically, is characterized by the degeneration or impairment of the neurons in the basal ganglia that produce dopamine. It’s this dopamine deficiency that directly causes movement-related problems. The actual cause of the damage to these neurons is not yet fully understood.
Parkinson’s is a brain disorder that results in unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination. 1 Symptoms usually begin gradually and worsen over time.
As the disease progresses, individuals might experience difficulty walking and talking. Mental and behavioral changes, sleep problems, depression, memory issues, and fatigue can also occur.
While anyone can be at risk for developing Parkinson’s, research suggests that it affects more men than women. The reasons for this are not yet clear, but research is being conducted to identify factors that might increase a person’s risk.
Age is a known risk factor: Although most people with Parkinson’s are diagnosed after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinson’s are sometimes, but not always, inherited, and some forms have been linked to specific genetic changes.
Understanding Parkinson’s Disease: Diagnosis and Treatment
Parkinson’s disease (PD) is a progressive neurological condition that affects movement and various other bodily functions. While there is currently no cure, early diagnosis, and effective treatment can significantly improve the quality of life for those living with the disease.
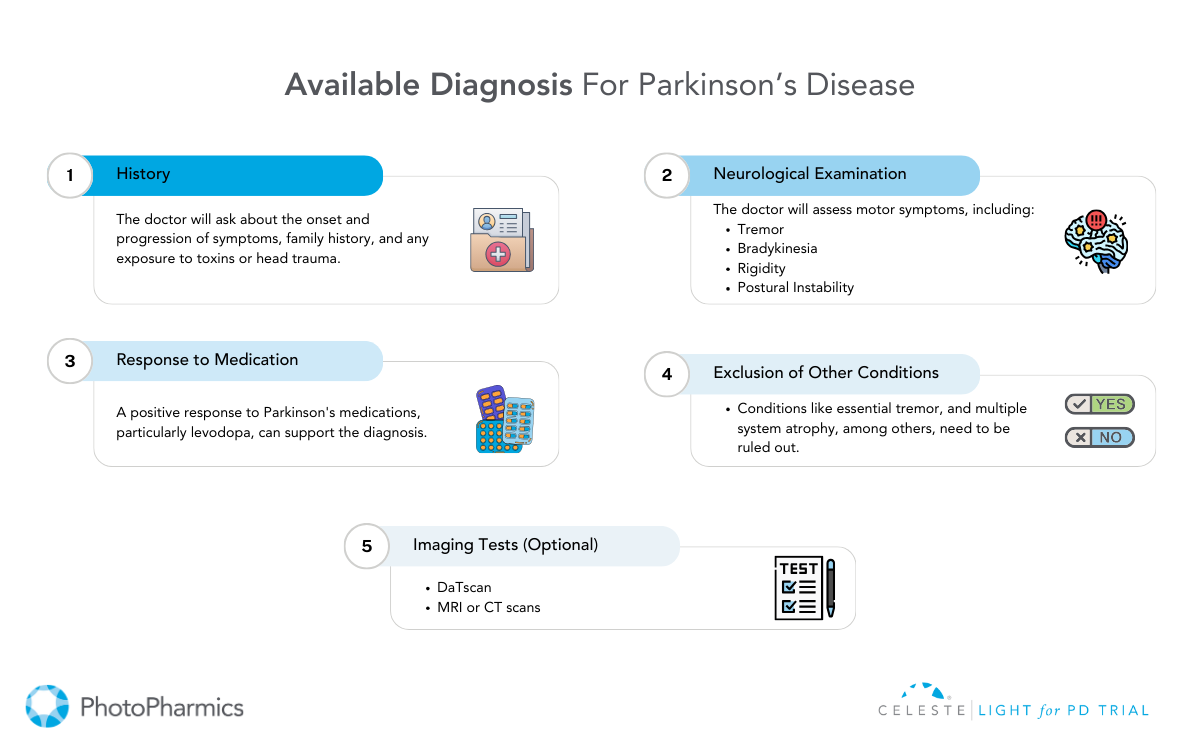
Diagnosing Parkinson’s Disease
Diagnosing Parkinson’s disease is primarily a clinical process. There is no single test that can confirm the condition. Instead, healthcare providers rely on a combination of medical history, symptom evaluation, and physical examinations. Laboratory and imaging tests are sometimes used to rule out other conditions that mimic Parkinson’s.
Common Diagnostic Approaches
- Medical History & Symptom Assessment: Doctors evaluate symptoms such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability.
- Neurological Examination: A detailed physical examination helps assess muscle stiffness, reflexes, coordination, and movement issues.
- Levodopa Response Test: If a patient’s symptoms improve with levodopa medication, it often confirms Parkinson’s.
Imaging and Laboratory Tests
While imaging and lab tests cannot diagnose Parkinson’s definitively, they help rule out other conditions. These include:
- Blood Tests: While not diagnostic for Parkinson’s, blood tests can help exclude other medical conditions that might be contributing to or mimicking the symptoms, such as thyroid problems or vitamin deficiencies.
- MRI & CT Scans: A CT scan uses X-rays to create cross-sectional images of the brain. It’s primarily used to visualize brain structures and rule out structural abnormalities like tumors or strokes that could be causing the symptoms.
- An MRI scan uses magnetic fields and radio waves to create detailed images of the brain. Like CT scans, MRIs help visualize brain structures and rule out other causes of symptoms. They can also sometimes help differentiate Parkinson’s from other neurodegenerative conditions.
- PET Scans: A PET scan uses a radioactive tracer to visualize brain activity. While not routinely used for Parkinson’s diagnosis, PET scans can sometimes help differentiate Parkinson’s from other conditions by showing patterns of brain activity. For example, a DaTscan, a type of PET scan, can visualize dopamine transporters in the brain and help confirm a diagnosis of Parkinsonian syndrome.
- Genetic Testing: Genetic testing may be considered in specific circumstances, such as early-onset Parkinson’s (diagnosed before age 50) or a strong family history of the disease. Certain genetic mutations are associated with an increased risk of Parkinson’s, though most cases are not directly linked to specific genes.
New Advances in Diagnostic Testing
- Spinal Tap (Lumbar Puncture): Researchers have found that analyzing cerebrospinal fluid for misfolded alpha-synuclein proteins may help in diagnosis.
- Skin Biopsy: A small sample of skin tissue is tested for abnormal alpha-synuclein deposits, which could indicate Parkinson’s disease.
Treatment and Management of Parkinson’s Disease
While Parkinson’s is incurable, various treatment strategies can help manage symptoms and enhance quality of life. Treatment plans are typically personalized based on symptom severity, progression, and individual response to therapy.
Medications for Parkinson’s Disease
Medications are the primary treatment for managing Parkinson’s symptoms. These fall into two main categories:
- Dopamine Replacement & Enhancement
- Levodopa: Levodopa is a precursor to dopamine and is converted into dopamine in the brain. It’s the most effective medication for managing motor symptoms, particularly bradykinesia and rigidity. However, long-term use can lead to motor fluctuations (on-off periods) and dyskinesia (involuntary movements).
- Levodopa-Carbidopa Combination: Carbidopa prevents levodopa from breaking down before reaching the brain, reducing side effects.
- Levodopa Metabolism Inhibitors: These medications, such as entacapone and tolcapone, prolong the effects of levodopa by inhibiting the enzyme COMT, which breaks down levodopa. They are typically used in combination with levodopa to manage motor fluctuations.
- Dopamine Agonists
- These medications mimic the action of dopamine in the brain, stimulating dopamine receptors. They can be used alone in early-stage Parkinson’s or in combination with levodopa. Common side effects include nausea, dizziness, sleepiness, and, in some cases, impulse control disorders.
- Other Medications
- Dopamine Metabolism Blockers: Help preserve dopamine levels in the brain.
- Adenosine Blockers: These medications, such as istradefylline, work on a different neurotransmitter system and can be used as an add-on therapy to levodopa to improve motor function.
- Amantadine: Helps reduce involuntary movements (dyskinesia).
- Anticholinergic Drugs: Assist in reducing tremors and muscle rigidity.
- MAO-B Inhibitors: These drugs block the enzyme monoamine oxidase B, which breaks down dopamine. By inhibiting this enzyme, MAO-B inhibitors help increase dopamine levels in the brain. They are often used in early-stage Parkinson’s or as an adjunct to levodopa.
Surgical Treatment: Deep Brain Stimulation (DBS)
For patients whose symptoms do not respond well to medication, Deep Brain Stimulation (DBS) is a surgical option.
- How it Works: Electrodes are implanted in specific brain areas and connected to a small device placed in the chest, which sends electrical impulses to regulate abnormal brain activity.
- Benefits: Reduces tremors, rigidity, and motor fluctuations, offering greater movement control.

Experimental Treatments & Future Research
Researchers are continuously exploring innovative treatments:
- Stem Cell Therapy: Aims to replace damaged neurons with healthy dopamine-producing cells.
- Neuron Repair Treatments: Focuses on regenerating and protecting nerve cells.
- Gene Therapy: Targets specific genetic mutations to slow disease progression.
- Light Therapy: Emerging research suggests that light therapy may help regulate circadian rhythms, improve sleep, and reduce non-motor symptoms in Parkinson’s patients.
Light for PD, a clinical trial by PhotoPharmics, explores how specialized light therapy can enhance the quality of life for individuals with PD.
Supportive Therapies and Lifestyle Management
Comprehensive care extends beyond medication and surgery. Supportive therapies can help patients maintain mobility, independence, and overall well-being.
- Physical Therapy: Enhances movement, flexibility, and strength.
- Occupational Therapy: Assists in daily activities and adaptive techniques.
- Speech Therapy: Helps with communication and swallowing difficulties.
- Dietary Changes: A balanced diet rich in fiber, antioxidants, and hydration supports overall health.
- Exercise & Alternative Therapies: Activities like yoga, tai chi, and massage therapy improve balance and flexibility.
If you or a loved one is affected by Parkinson’s, consult with a healthcare professional to explore the best treatment options
On Stable Meds But Still Not Satisfied?
Research continues to explore new therapies, including gene therapy, neuroprotective drugs, and innovative treatments like light therapy.
A promising investigational FDA Breakthrough device, “Celeste,” is in the clinical trials, being developed to improve both motor and non-motor symptoms in Parkinson’s disease. This at-home light therapy device aims to enhance quality of life beyond current medications.

Why Join the Trial?
- No travel or medication changes are required.
- Open to anyone with Parkinson’s in the U.S.
- Convenient, and used during daily activities.
- No cost to participants—they receive $500 for completing the trial.
Is There a Better Way to Manage PD Symptoms?
Many people with PD experience lingering symptoms like fatigue, sleep issues, and anxiety.
Celeste offers a non-drug alternative designed to address these unmet needs. Learn more and see if you qualify for the Celeste Light for PD Trial today!
Introduction
The tremor. The stiffness. The deliberate slowness of movement. These are the hallmarks often associated with Parkinson’s disease.
But what if these very same symptoms point to something else entirely?
This is the complex reality of Parkinsonism. It encompasses a range of conditions that mimic Parkinson’s disease, creating diagnostic challenges for even experienced clinicians.
While slowness (bradykinesia), rigidity, and resting tremor are key indicators, they are not exclusive to Parkinson’s disease.
This diagnostic overlap necessitates careful evaluation by a neurologist to distinguish between Parkinson’s disease and other forms of Parkinsonism.
What makes Parkinsonism particularly complex is its ability to mimic Parkinson’s disease, creating challenges in pinpointing the exact cause of symptoms.
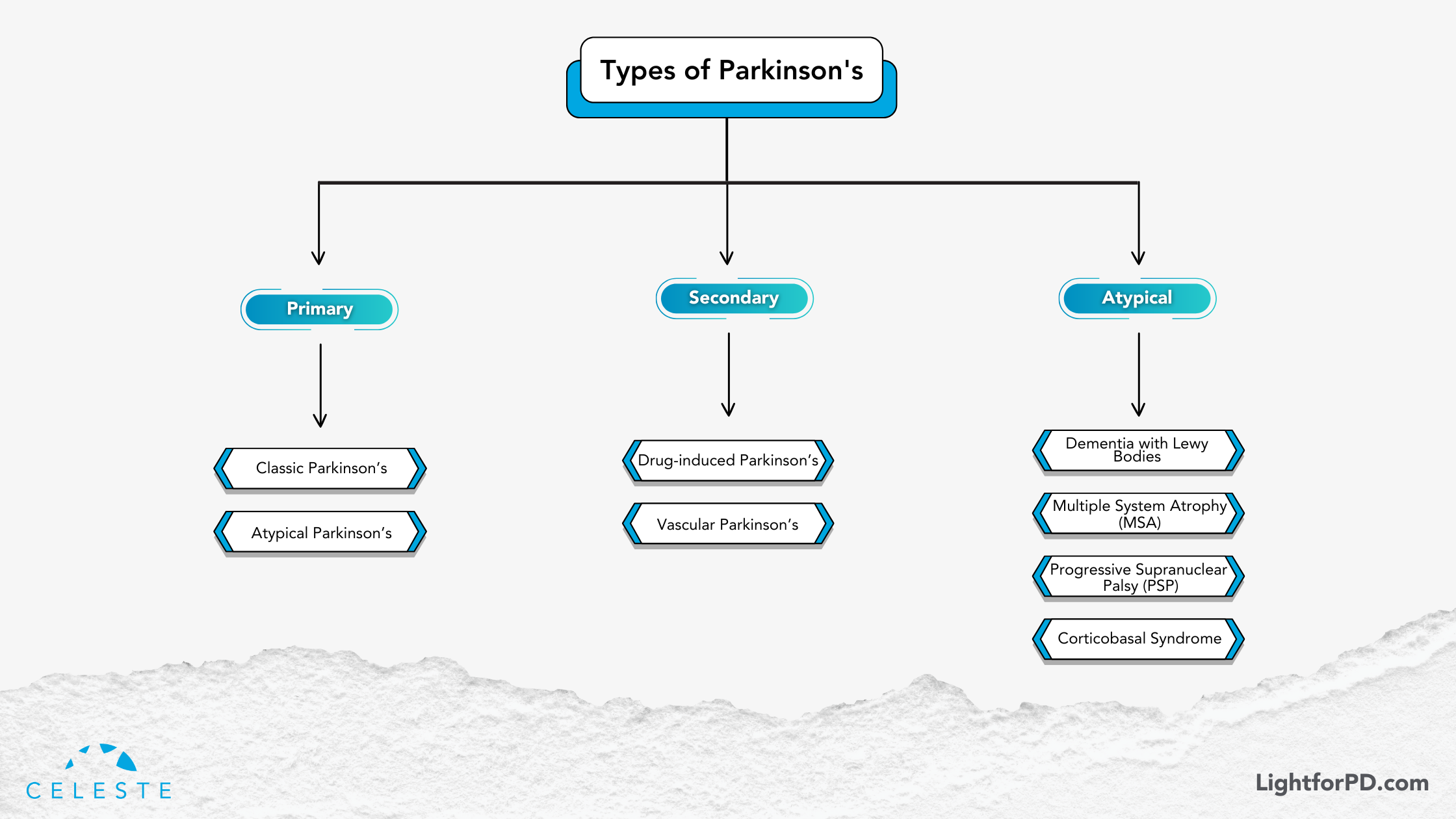
It’s important to understand that Parkinsonism is not a single disease but rather a spectrum of disorders categorized as primary and secondary.
In this blog, we’ll explore the most common conditions associated with Parkinsonian symptoms, shedding light on their differences and helping you navigate this intricate topic with greater clarity.
Whether you’re a patient, caregiver, or simply curious, this guide will give you a deeper understanding of the types of Parkinsonism and their unique characteristics.
Parkinsonism Classification
Parkinsonism is broadly categorized into two main types: primary and secondary. Let’s explore each in detail.
Primary Parkinsonism
Primary Parkinsonism refers to conditions where the underlying cause is a neurodegenerative process—a gradual decline in specific brain cells. This category includes PD itself, as well as a group of related disorders known as atypical Parkinsonian disorders.
Parkinson’s Disease (PD)
This is the most common form of Parkinsonism. It’s characterized by the progressive loss of dopamine-producing neurons in the brain. This leads to classic motor symptoms: tremors at rest, bradykinesia (slowness of movement), rigidity (stiffness), and postural instability (balance problems). PD typically responds well to levodopa, a medication that converts to dopamine in the brain, replenishing the depleted stores.

Atypical Parkinsonian Disorders
These conditions share some symptoms with PD but have distinct features and often respond differently to treatment. They include:
- Dementia with Lewy Bodies (DLB): This disorder is characterized by the presence of Lewy bodies (abnormal protein deposits) in the brain, similar to those found in PD but with a different distribution. In addition to motor symptoms, DLB is marked by fluctuating cognition, visual hallucinations, and REM sleep behavior disorder. Levodopa may offer some benefit for motor symptoms, but often less effectively than in PD, and can sometimes worsen psychiatric symptoms.
- Progressive Supranuclear Palsy (PSP): PSP is characterized by early balance problems with frequent falls, difficulty with eye movements (especially looking downwards), rigidity in the neck and upper body, and cognitive changes. Unlike PD, tremor is usually not prominent in PSP. Levodopa typically provides minimal relief.
- Multiple System Atrophy (MSA): MSA is a rapidly progressive disorder affecting multiple systems in the body, including the autonomic nervous system (which controls involuntary functions like blood pressure and digestion), the cerebellum (which coordinates movement), and the basal ganglia (involved in motor control). Symptoms vary depending on the specific systems affected but can include parkinsonism, cerebellar ataxia (problems with balance and coordination), autonomic dysfunction (e.g., dizziness, bladder problems), and speech difficulties. Levodopa is generally not very effective in managing MSA.
- Corticobasal Degeneration (CBD): CBD is a rare disorder characterized by progressive motor and cognitive decline. Motor symptoms can include rigidity, dystonia (sustained muscle contractions), apraxia (difficulty with skilled movements), and alien limb phenomenon (involuntary movements of a limb). Cognitive changes can include problems with language, executive function, and visuospatial skills. Levodopa is usually not helpful in CBD.
Secondary Parkinsonism: When External Factors Play a Role
Secondary Parkinsonism arises from identifiable external factors, such as medications, toxins, or other medical conditions. Unlike primary Parkinsonism, the symptoms may be reversible if the underlying cause is addressed.
- Drug-Induced Parkinsonism: Certain medications, particularly antipsychotics, can block dopamine receptors in the brain, leading to Parkinsonian symptoms. These symptoms usually resolve when the medication is stopped.
- Vascular Parkinsonism: This type of Parkinsonism results from small strokes or other vascular problems in the brain that affect the areas responsible for motor control. Symptoms can be more variable than in PD and may include lower-body parkinsonism (affecting mainly the legs). Levodopa is typically not effective.
Other Secondary Causes: Other potential causes of secondary Parkinsonism include head trauma, infections, and exposure to certain toxins.
The Levodopa Response: A Key Differentiator
A crucial distinction between PD and many other forms of Parkinsonism is the response to levodopa. While PD typically shows a good initial response to this medication, atypical Parkinsonian disorders and secondary Parkinsonism often show little or no improvement. This difference can be a valuable clue for clinicians in making a diagnosis.
The Importance of Accurate Diagnosis
Differentiating between PD and other forms of Parkinsonism is essential because each condition has a different prognosis and requires tailored management strategies. A neurologist, especially one specializing in movement disorders, is best equipped to make an accurate diagnosis through a thorough neurological examination, medical history review, and sometimes brain imaging.
This information is intended for educational purposes and should not be considered medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Diagnosing Parkinson’s Disease
Diagnosing Parkinson’s disease (PD) is a complex process. It’s a clinical puzzle that clinicians piece together using a combination of careful observation, detailed medical history, and neurological examination.
Unlike many other diseases, there is no single definitive test, such as a blood test or brain scan, that confirms a PD diagnosis.
The absence of a “gold standard” biomarker requires diagnosis to focus on motor symptoms while excluding similar conditions.
This clinical diagnostic approach can present challenges, especially in the early disease stages when symptoms are subtle or overlap with other conditions.
This reliance on clinical observation has driven the development and refinement of diagnostic criteria over time.

Evolving Diagnostic Standards
Historically, diagnostic criteria like those from the U.K.’s Parkinson’s Disease Society Brain Bank provided a framework for clinicians.
However, our understanding of PD has evolved significantly, leading to the adoption of newer, more refined criteria from the International Parkinson and Movement Disorder Society.
These updated standards reflect the latest research and clinical insights, aiming to improve diagnostic accuracy and enable earlier intervention.
The core motor symptoms clinicians look for include: resting tremor (a trembling that occurs when the limb is at rest), bradykinesia (slowness of movement), rigidity (muscle stiffness), and postural instability (balance problems).
These cardinal features, when present in combination and carefully assessed, form the cornerstone of a PD diagnosis.
Beyond the Motor Symptoms: Exploring Prodromal Markers and Advanced Imaging
While motor symptoms are central to diagnosis, researchers are increasingly recognizing the importance of non-motor symptoms. These symptoms are often referred to as prodromal markers, which can precede the onset of motor difficulties by years.
These subtle clues, such as loss of smell (anosmia), REM sleep behavior disorder (acting out dreams), constipation, and mood changes like depression or anxiety, are being investigated as potential early indicators of PD risk.
Additionally, while not diagnostic on their own, advanced imaging techniques like the DaTscan can provide valuable supporting evidence. The DaTscan uses a radioactive tracer to visualize dopamine transporter activity in the brain. It helps to differentiate PD from other conditions with similar motor presentations.
This technology allows clinicians to see if the reduction in dopamine transporter activity is consistent with PD, further strengthening the diagnostic picture.
Ongoing research into biomarkers holds the promise of even earlier and more precise diagnostic tools in the future. This will potentially allow for earlier interventions to slow disease progression.
A Brighter Future: Exploring Light Therapy for Non-Motor Symptoms
Beyond the motor challenges of Parkinson’s, non-motor symptoms such as sleep disturbances, mood disorders, and fatigue can significantly impact quality of life. As research advances in diagnosing Parkinson’s, innovative approaches are also emerging to help manage the condition’s impact.
For instance, Light for PD (our ongoing Parkinson’s clinical trial) is exploring the benefits of light therapy for managing non-motor symptoms of Parkinson’s. This non-invasive, at-home therapy offers a promising option to improve the quality of life for those living with PD. By targeting symptoms such as sleep disturbances and mood changes, Light for PD provides a gentle, science-backed way to complement existing treatment plans. If you or someone you know is navigating Parkinson’s, consider joining this trial to explore a new pathway to relief.
For more information to check your eligibility, visit www.lightforpd.com.