Introduction
Imagine waking up after a full night’s sleep, yet feeling as though you haven’t slept in days. Your limbs feel heavy, as if you are moving through molasses, and the mental effort required to simply plan your day feels akin to solving complex calculus.
This is not the “tiredness” that follows a long day of work or a rigorous gym session. This is Parkinson’s disease (PD) fatigue—a symptom that is as enigmatic as it is debilitating.
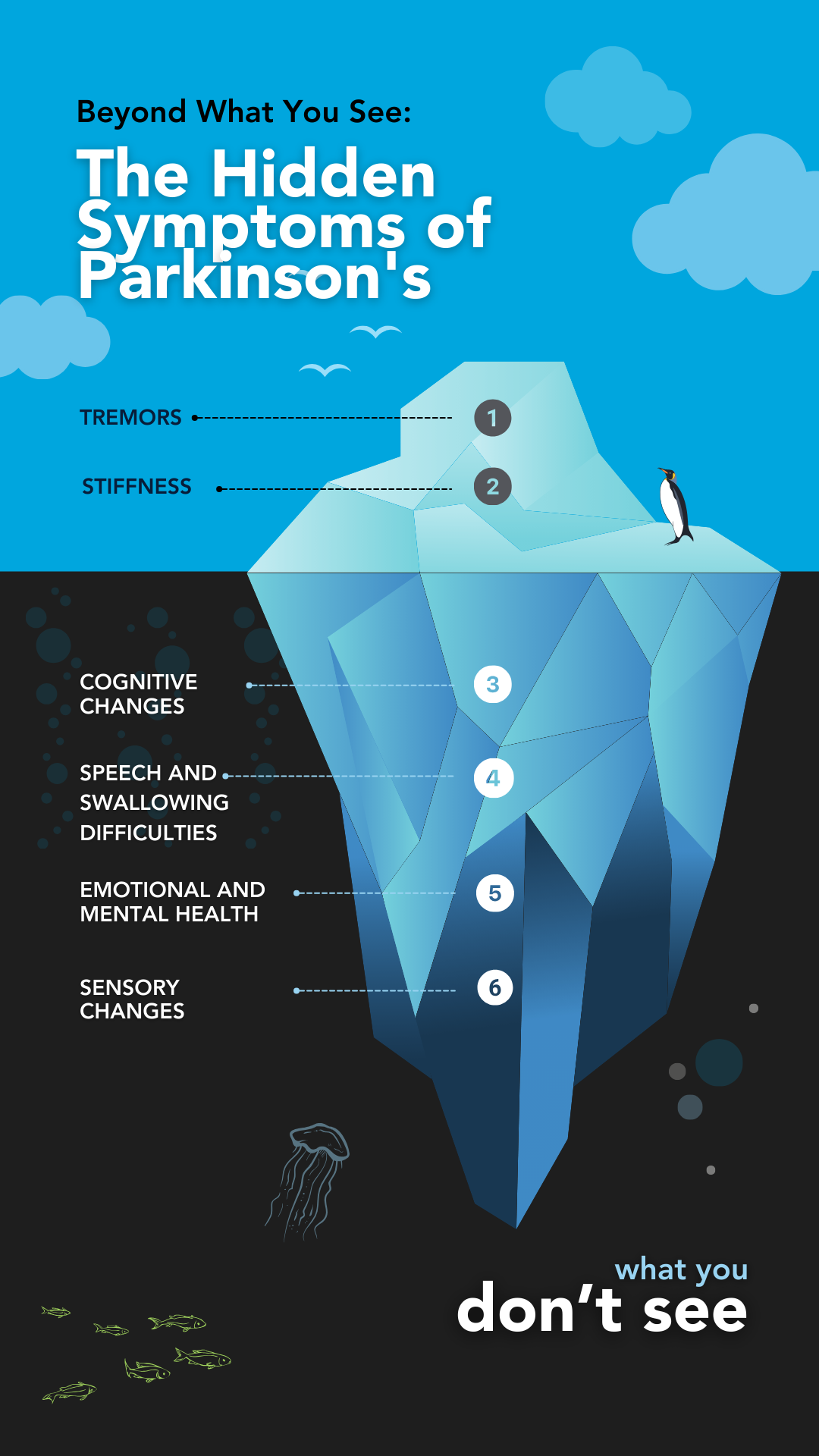
For decades, the public focus on Parkinson’s has centered on the visible motor symptoms: the tremors, the stiffness, and the shuffling gait.
However, for those living with the condition, the reality is often quite different. Studies consistently show that fatigue affects between 33% and 81% of patients, with nearly one-third citing it as their single most disabling symptom. It is an overwhelming sense of exhaustion that encompasses both physical and mental domains, often disproportionate to the activity undertaken and frequently unalleviated by rest.
Crucially, fatigue is not a sign of laziness, depression, or a simple lack of sleep. It is a primary physiological manifestation of the disease itself—a signal that the neurodegenerative process is affecting networks far beyond those that control movement.
By peeling back the layers of neurobiology, inflammation, and metabolic failure, we can begin to validate this invisible struggle and, more importantly, find strategic ways to manage it. This article explores the deep science behind why fatigue occurs and offers evidence-based strategies to reclaim your energy.
Fatigue: More Than Just Being “Tired”
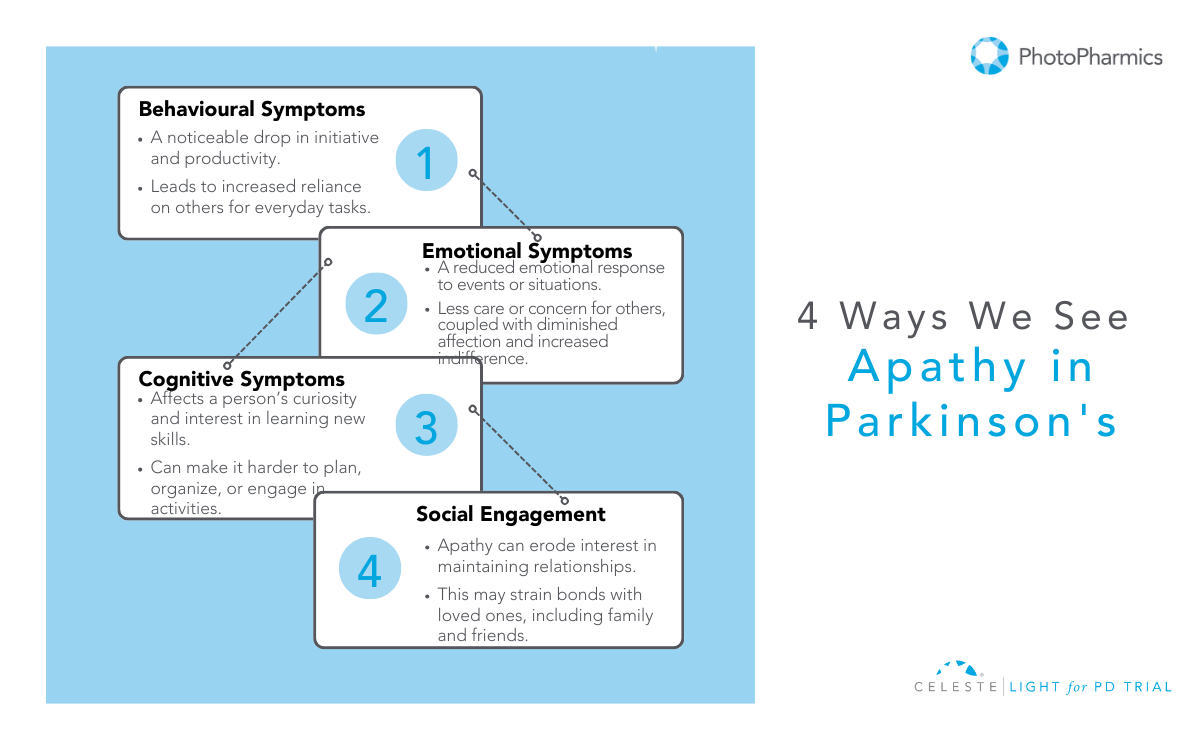
To manage fatigue, we must first define it accurately. In the clinical landscape of Parkinson’s, fatigue is a distinct entity, separate from sleepiness (somnolence) or a lack of interest (apathy), though they often overlap.
Fatigue in PD is multidimensional. Patients often describe a “failure to initiate”—a sensation where the brain knows what to do, but the body simply cannot muster the energy to execute the command. This is known as Subjective Fatigue. It is a central sensation, a perception of weariness that acts as a heavy cloak over daily life.
Interestingly, this internal feeling doesn’t always match muscle performance. You might feel too weak to walk, but your muscles are physiologically capable of the task.
Contrast this with Objective Fatigability, which is a measurable decline in performance. In PD, this is “peripheral” fatigability. If you were to perform a repetitive motion, your force generation would decline more rapidly than that of a healthy person. This creates a frustrating disconnect: a central nervous system that struggles to drive the muscle, combined with muscles that tire too quickly.
Furthermore, the fatigue is pleiotropic, meaning it affects multiple systems. There is Physical Fatigue, characterized by muscle weakness and kinetic exhaustion, and Mental Fatigue, a difficulty in sustaining attention or concentration.
The latter is particularly intrusive, making tasks that require executive function—like balancing a checkbook or following a conversation—feel like climbing a mountain.
Understanding these distinctions is the first step toward targeted management.

The Science Behind Fatigue in Parkinson’s
Why does the brain stop generating energy?
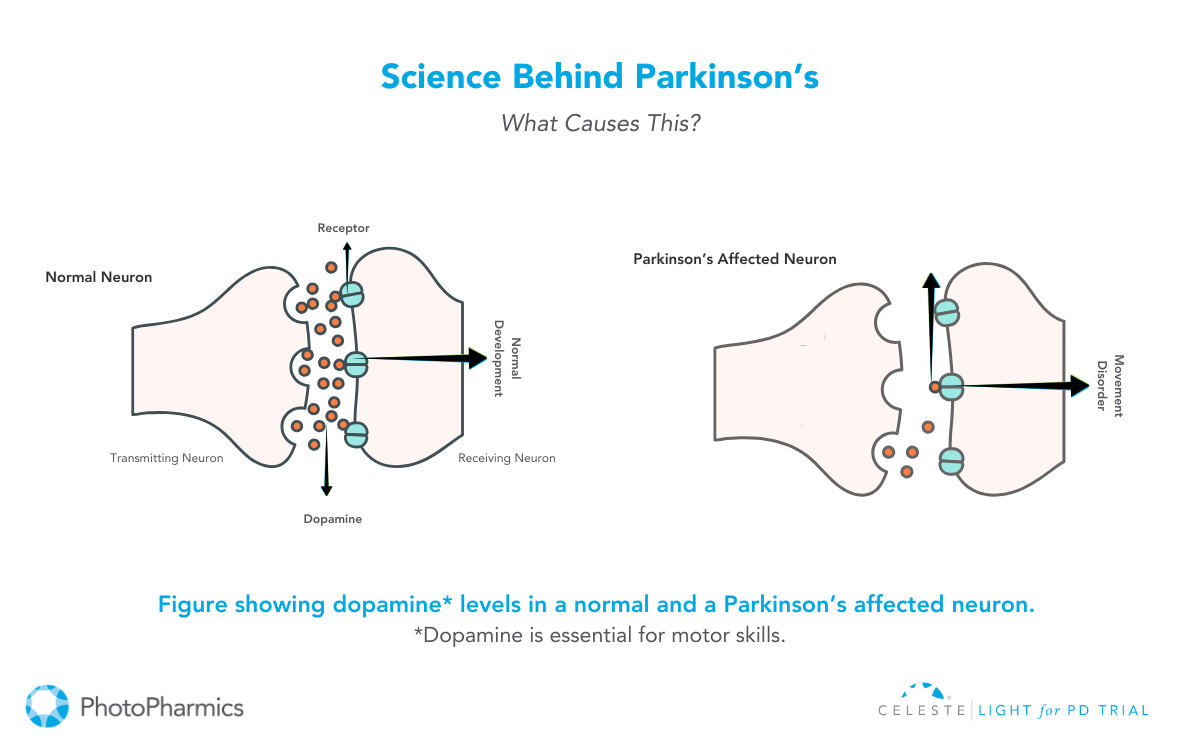
One of the most compelling neurobiological theories is the Effort-Reward Imbalance Hypothesis.
Every action we take, from reaching for a coffee cup to walking to the mailbox, involves a split-second calculation by the brain: Is the reward of this action worth the effort required to achieve it? This calculation relies heavily on dopamine, particularly in the mesolimbic system—the brain’s reward center.
In Parkinson’s, the degeneration of dopamine-producing neurons isn’t limited to the areas controlling movement (the nigrostriatal pathway). It extends to the ventral tegmental area, which projects to the nucleus accumbens. When dopamine is depleted here, the brain’s “currency converter” breaks down.
The result is a skewed cost-benefit analysis. The brain begins to inflate the perceived “cost” (effort) of an action while diminishing the perceived “value” of the reward. To the PD brain, walking to the kitchen might “cost” as much energy as running a mile, while the reward of getting a glass of water feels negligible.
Consequently, the sensation of fatigue acts as a behavioral “stop signal.” It is the brain’s misguided attempt to conserve energy because it calculates that the exertion isn’t justified. This “central activation deficit” means patients have to exert massive mental willpower to override this stop signal, leading to profound exhaustion.
Additionally, this isn’t just about dopamine. Serotonin, the neurotransmitter regulating mood and sleep, plays a massive role. Serotonergic neurons in the brainstem often degenerate before dopamine neurons. PET scan studies reveal that fatigued PD patients have significantly reduced serotonin transporter availability in the limbic system.
This explains why fatigue often persists even when patients are perfectly medicated with Levodopa—the dopaminergic deficit is treated, but the serotonergic “non-dopaminergic” fatigue remains.
Inflammation and “Sickness Behavior”
While the brain struggles with neurotransmitters, the body is fighting its own battle. Emerging research supports a “whole-body” view of PD fatigue, suggesting it mimics “sickness behavior”—the lethargy you feel when you have the flu.
Parkinson’s is increasingly viewed as a state of chronic, low-grade inflammation. Patients often exhibit elevated levels of pro-inflammatory cytokines, specifically Interleukin-6 (IL-6) and Tumor Necrosis Factor-alpha (TNF-alpha). These inflammatory messengers don’t just stay in the blood; they cross the blood-brain barrier and activate microglia, the brain’s immune cells.
When microglia are activated, they release reactive oxygen species and more cytokines, creating a toxic, inflammatory environment that impairs neural signaling. This biological state signals the body to withdraw, rest, and conserve energy to “fight” an infection that isn’t actually there.
A key player in this process is the NLRP3 inflammasome, an intracellular alarm system. In a healthy brain, dopamine inhibits this alarm. But in PD, as dopamine levels fall, the “brake” on the immune system is removed. The NLRP3 inflammasome becomes hyperactive, churning out inflammatory signals that drive fatigue.
Simultaneously, there is a crisis in the cellular power plants: the mitochondria. A systemic reduction in Complex I activity of the mitochondrial electron transport chain is a robust finding in PD. This means the cells are literally less efficient at producing ATP, the energy currency of life. This bioenergetic failure is systemic, found in skeletal muscles as well as the brain, explaining why physical endurance is so compromised.
Factors Contributing to Fatigue
If neurodegeneration and inflammation are the core of the onion, secondary comorbidities are the outer layers. These are often the most treatable aspects of fatigue, yet they frequently go diagnosing.
Sleep Pathology is ubiquitous. It’s not just about getting eight hours; it’s about the quality of that sleep. Many PD patients suffer from Obstructive Sleep Apnea (OSA) or REM Sleep Behavior Disorder (RBD), where they physically act out dreams. This fragmentation prevents restorative sleep, leaving the brain in a permanent state of debt.
Autonomic Dysfunction is another silent thief of energy. Many patients experience Neurogenic Orthostatic Hypotension (nOH)—a drop in blood pressure upon standing. This happens because the autonomic nervous system fails to release enough norepinephrine to constrict blood vessels. The result is chronic cerebral hypoperfusion. Even if you don’t faint, your brain is getting slightly less oxygen than it needs whenever you are upright. This manifests as “brain fog,” visual blurring, and a coat-hanger ache in the neck and shoulders—all perceived as profound tiredness.
Finally, we must address Neuropsychiatric Factors. While depression and fatigue are distinct, they feed into each other. Depression can rob a patient of motivation (anhedonia), while apathy—a lack of interest separate from sadness—can mimic the “effort-reward” failure of fatigue. Distinguishing these requires careful clinical assessment, as the treatment for depression (SSRIs/SNRIs) differs from the treatment for pure fatigue or apathy.

Pharmacological Management: Consult Your Doctor
When it comes to treating fatigue with medication, the landscape is complex and highly individualized. There are numerous pharmaceutical options available today that target different aspects of fatigue—whether it stems from dopamine deficiency, excessive daytime sleepiness, or other underlying chemical imbalances.
However, because fatigue in Parkinson’s is so multifaceted—involving everything from neurotransmitters to blood pressure regulation—no single drug works for everyone.
What provides energy for one patient might cause side effects in another.
Therefore, it is absolutely essential to have a detailed conversation with your neurologist or movement disorder specialist. They can help identify the specific type of fatigue you are experiencing and tailor a treatment plan that is safe and effective for your unique medical profile.
Exercise: The Only Disease-Modifying Strategy?
While pills treat symptoms, exercise may actually change the biology of the fatigued brain. It is arguably the most robust intervention available.
Aerobic Training is critical. Regular cardiovascular exercise (walking, cycling, swimming) does more than just strengthen the heart; it lowers the resting levels of those pro-inflammatory cytokines (IL-6) that drive sickness behavior. It also improves oxygen delivery to the mitochondria, helping to mitigate the bioenergetic failure.
However, intensity matters. Emerging research on High-Intensity Interval Training (HIIT) suggests that pushing your heart rate to 60-80% of its reserve triggers the release of Brain-Derived Neurotrophic Factor (BDNF). BDNF acts like fertilizer for the brain, promoting synaptic plasticity in the basal ganglia. High-intensity work has also been shown to normalize “cortical silent periods”—essentially resetting the excitability of the motor cortex.
Resistance Training is the other half of the equation. By increasing muscle strength, you lower the relative effort required for daily tasks. If your legs are stronger, standing up from a chair takes 30% of your maximum effort instead of 80%, leaving you with more energy in the tank for the rest of the day.
The recommended prescription is a mix: at least 3 days a week of aerobic activity combined with resistance training, totaling 30-40 minutes per session.

Diet and Lifestyle Management
Finally, management extends to how you fuel your body and how you spend your energy budget.
From a dietary perspective, metabolic therapies are gaining traction. A randomized trial comparing a Mediterranean diet to a Ketogenic diet found that while both improved health, the Ketogenic group (high fat, low carb) saw significantly greater improvements in non-motor symptoms like fatigue.
The theory is that ketone bodies can bypass the defective Complex I in the mitochondria, providing an alternative, more efficient fuel source for neurons. While a strict Keto diet is hard to maintain, moving toward a lower-carb, healthy-fat diet may offer benefits.
Fatigue in Parkinson’s is a heavy burden, impacting not just the patient but the entire family unit. It limits social interaction and increases caregiver strain.
But by recognizing it as a physiological storm—of inflammation, neurochemistry, and metabolism—we can stop blaming ourselves and start managing our biology.
Through a combination of smart medication, high-intensity movement, and strategic energy budgeting, vitality is not a thing of the past.
Understanding Parkinson’s is a journey of continuous discovery. To stay updated on the latest news, insightful information, and updates regarding Parkinson’s research and management follow @photopharmics_ on social media.
Introduction
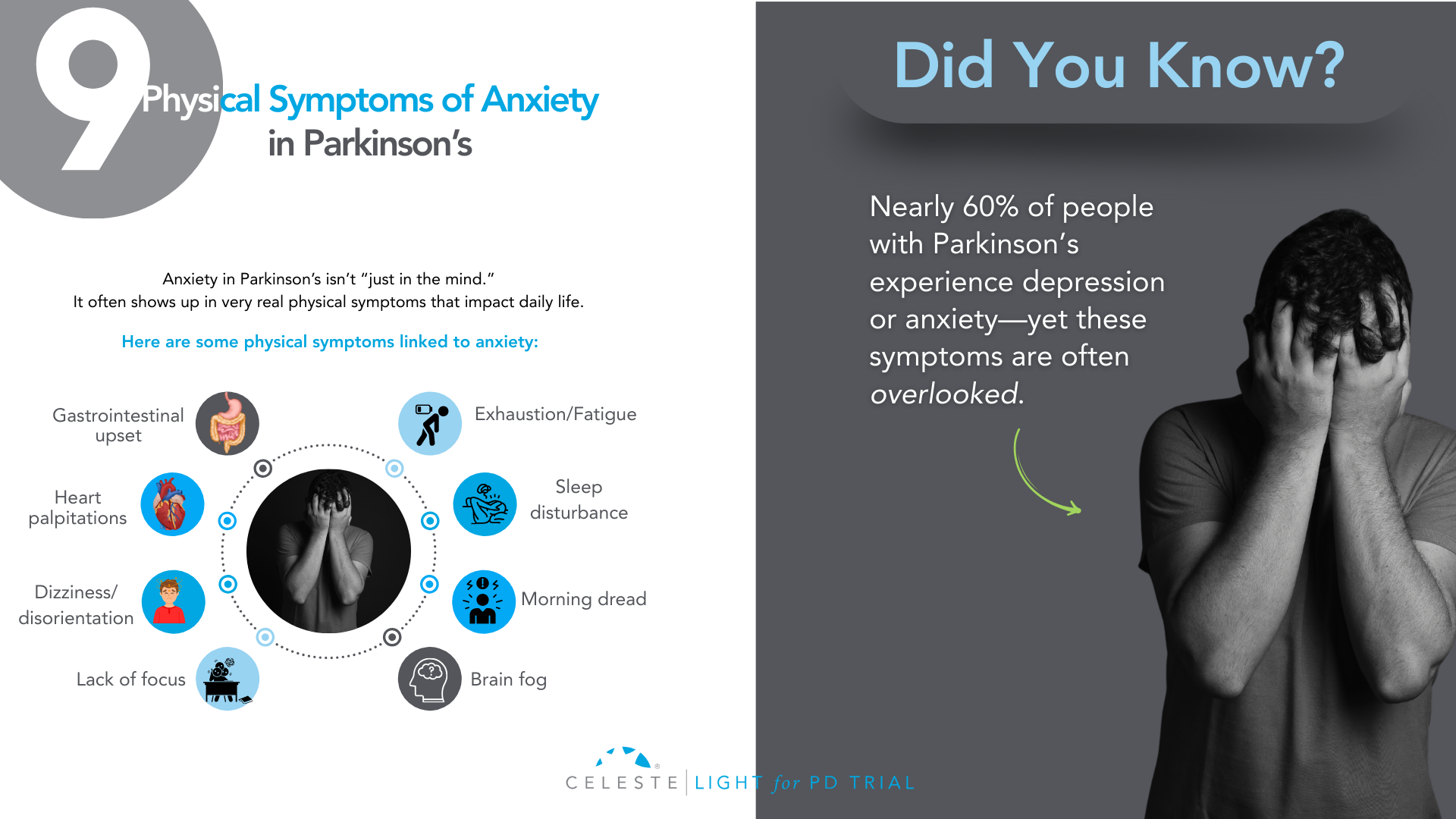
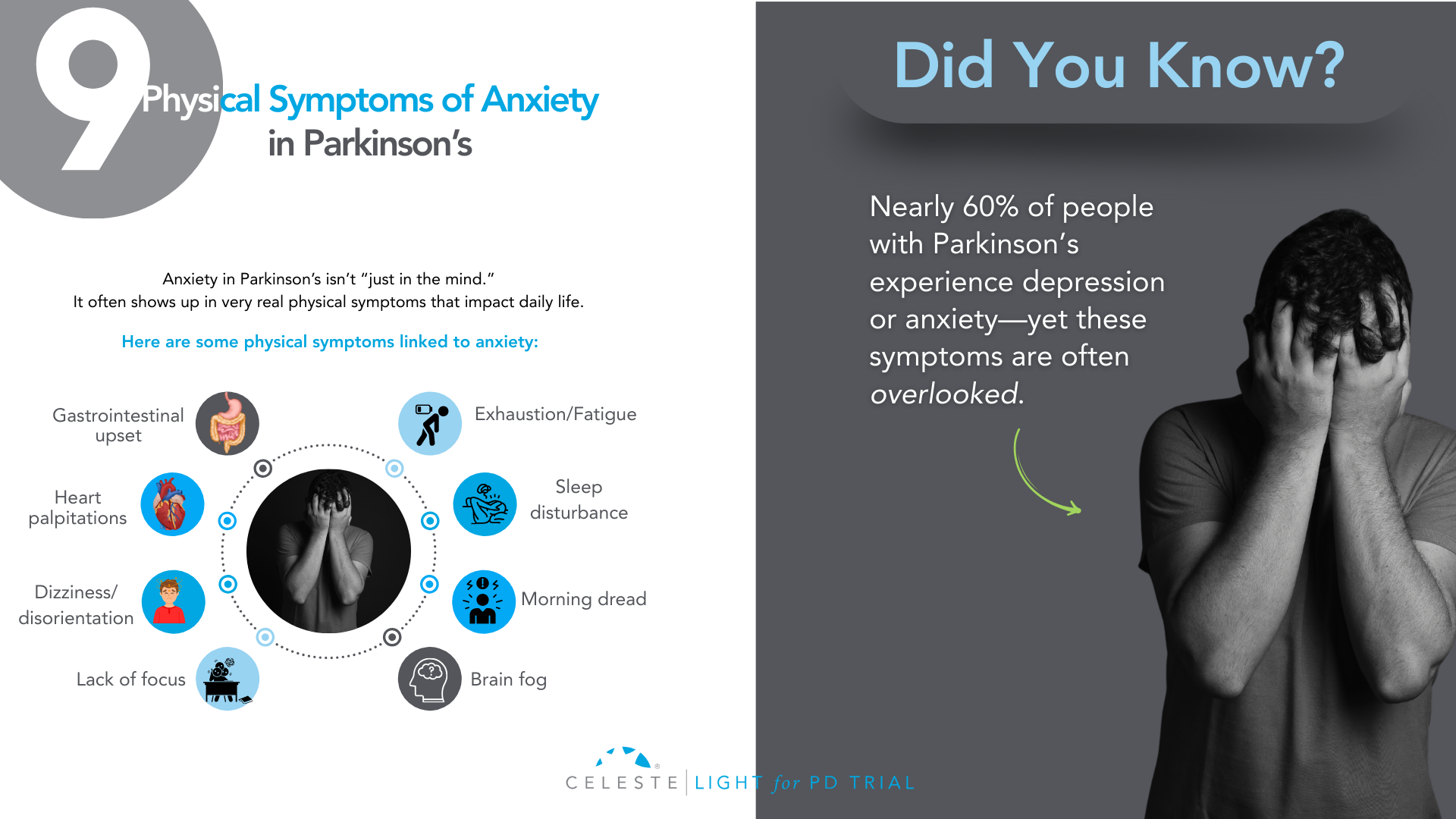
Did you know that at least 50% of people with Parkinson’s Disease (PD) will experience some form of depression during their illness, and up to 40% will face a significant anxiety disorder?
If you’ve been grappling with your mood, you are far from alone. For too long, the conversation around Parkinson’s has focused almost exclusively on the visible, motor symptoms like tremor, stiffness, and slowness.
But as you know, that’s only part of the story. The invisible challenges—the ones that happen inside—are often the heaviest to carry.
Many people, including doctors in the past, assumed that feeling down or anxious was just a natural emotional reaction to being diagnosed with a chronic illness.
While that can certainly be a factor, we now understand something much more profound: depression and anxiety are a core, biological part of the disease itself.
The same changes happening in your brain that affect movement are also affecting the chemistry of your mood.
This isn’t just a side issue; for many, it’s the main issue. It’s the hidden struggle that can impact your quality of life even more than the physical symptoms.
But here is the most important message: it is treatable. You do not have to “just live with it.”
This guide will walk you through this. We will explore why these feelings happen and look at what they look like in PD. This guide will discuss their impact on you and your loved ones. Most importantly, we will cover effective treatments. We will show strategies that can help you. You can reclaim your well-being.
The Celeste (Light for PD) trial shows promising results with a non-invasive approach to managing depression in Parkinson’s. Early findings point toward better support and improved quality of life. Find out how you can get involved.
Why Mood Changes Are Part of Parkinson’s?
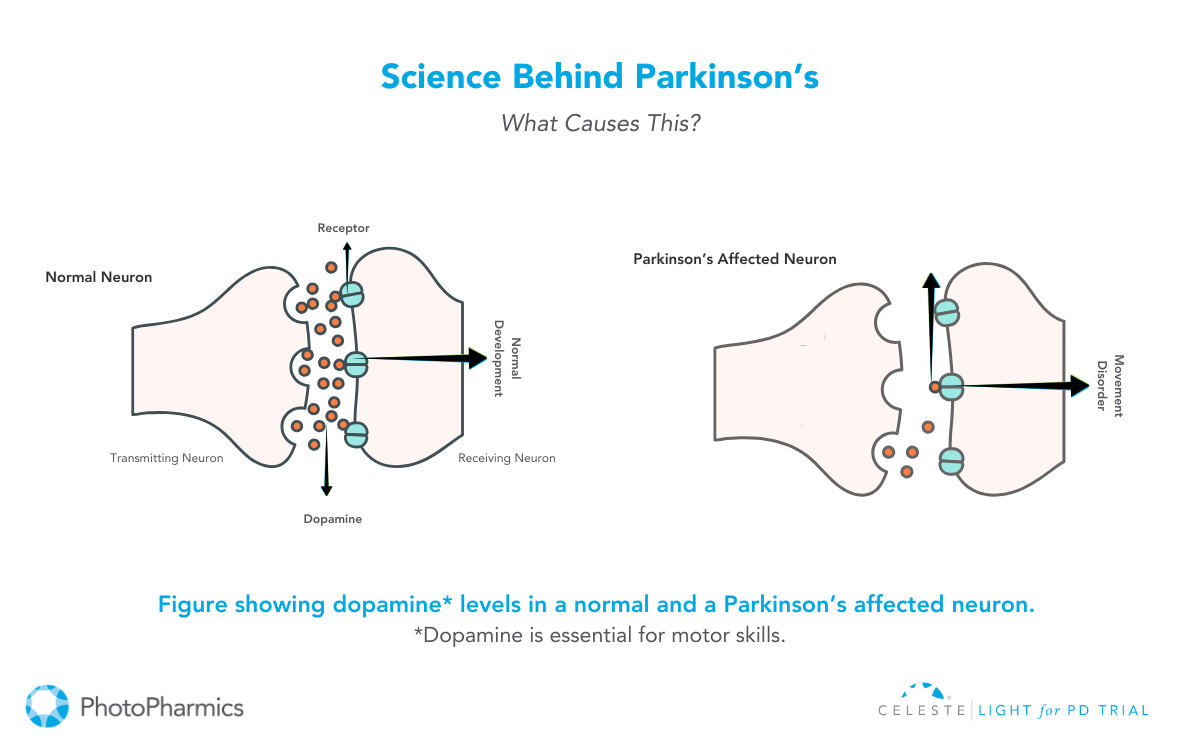
To understand why mood changes are so common in Parkinson’s, we need to look beyond dopamine.
While PD is mainly caused by a loss of dopamine-producing cells, this is just one piece of a much bigger puzzle. The neurodegenerative process affects other crucial brain chemical systems as well. Think of it as a “neurotransmitter triad” involving dopamine, serotonin, and norepinephrine.
Role of Neurotransmitters
- Dopamine: This chemical is famous for its role in movement, but it’s also fundamental to our brain’s reward and motivation system. When the dopamine pathways that govern pleasure and drive are damaged, it can lead directly to apathy (a lack of motivation) and anhedonia (the inability to feel pleasure), which are core symptoms of depression.
- Serotonin: This is perhaps the most well-known mood-regulating chemical. The brain changes in PD also cause a significant loss of serotonin-producing neurons. This isn’t a side effect. It’s a direct hit on the system that helps keep our mood stable, our anxiety in check, and our sleep regulated. This direct link is a major reason why depression is so prevalent in PD.
- Norepinephrine: This chemical is essential for energy, focus, and our response to stress. The part of the brain that produces norepinephrine is also significantly affected in Parkinson’s. A drop in this chemical can contribute to the profound fatigue that so many experience, as well as to both depression and anxiety.
This complex, multi-system chemical imbalance explains so much. It tells us that what you’re feeling is real and has a physical cause. It also highlights one of the most compelling pieces of evidence: depression and anxiety often show up before any motor symptoms appear, sometimes by several years.
This strongly suggests that the mood-regulating parts of the brain are among the first to be affected by the disease process. Recognizing this can be empowering. It reframes your emotional struggles from a personal failing into a manageable symptom of your condition, just like a tremor or stiffness.

What Does Depression and Anxiety Look Like in Parkinson’s?
One of the biggest hurdles to getting help is that depression and anxiety don’t always look the way you’d expect, especially with Parkinson’s in the picture. There’s a significant and confusing overlap between the symptoms of PD and the symptoms of a mood disorder.
This clinical mimicry is a major reason why mood disorders are so often missed. You might feel fatigued and assume it’s “just the Parkinson’s.” Your family might see your reduced facial expression (hypomimia or “masked face”) and think you’re withdrawn or disinterested, when in reality it’s the PD affecting your facial muscles.
This is why it’s so critical to talk specifically about how you’re feeling on the inside, not just what’s showing on the outside.
Let’s break down how these conditions can manifest:
Depression in Parkinson’s can include:
- Major Depressive Disorder: This is what most people think of as clinical depression, involving a persistent low mood, loss of interest or pleasure, and other symptoms that make it hard to function.
- Minor Depression or Dysthymia: This is actually more common in PD. You may not meet the full criteria for major depression, but you experience a chronic, low-grade sadness and other depressive symptoms that still significantly impact your quality of life.
- Intense Feelings of Despair: We need to address this with care and honesty. For some, depression can lead to intense feelings of despair and even thoughts of not wanting to be alive anymore. If you ever find yourself having these thoughts, it is a medical emergency and a sign that the depression has become severe. Please understand that these thoughts are a symptom of the illness, and they can be treated. It is crucial that you reach out for help immediately—contact your doctor, a support hotline, or a trusted person in your life without delay.
The Celeste (Light for PD) trial shows promising results in addressing depression in Parkinson’s. This innovative research is exploring an innovative and non-invasive approach to improve your parkinson’s symptoms. Learn more and see if participation is right for you.

- Generalized Anxiety Disorder (GAD): This is a state of constant, excessive worry and nervousness that you can’t control. It can be accompanied by physical symptoms like a racing heart, sweating, or even a worsening of your tremor.
- Panic Attacks: These are sudden, intense episodes of overwhelming fear. In PD, they are often linked to medication “off” periods, when your motor symptoms return as your medication wears off. This can be terrifying, making you feel like you’re having a heart attack or can’t breathe.
- Social Phobia: This is an intense fear of being embarrassed or judged in social situations. It’s often driven by self-consciousness about visible symptoms like tremor, walking difficulties, or dyskinesias. This can lead to avoiding friends and family, causing profound isolation.
How Mood Impacts Your Life and Your Family?
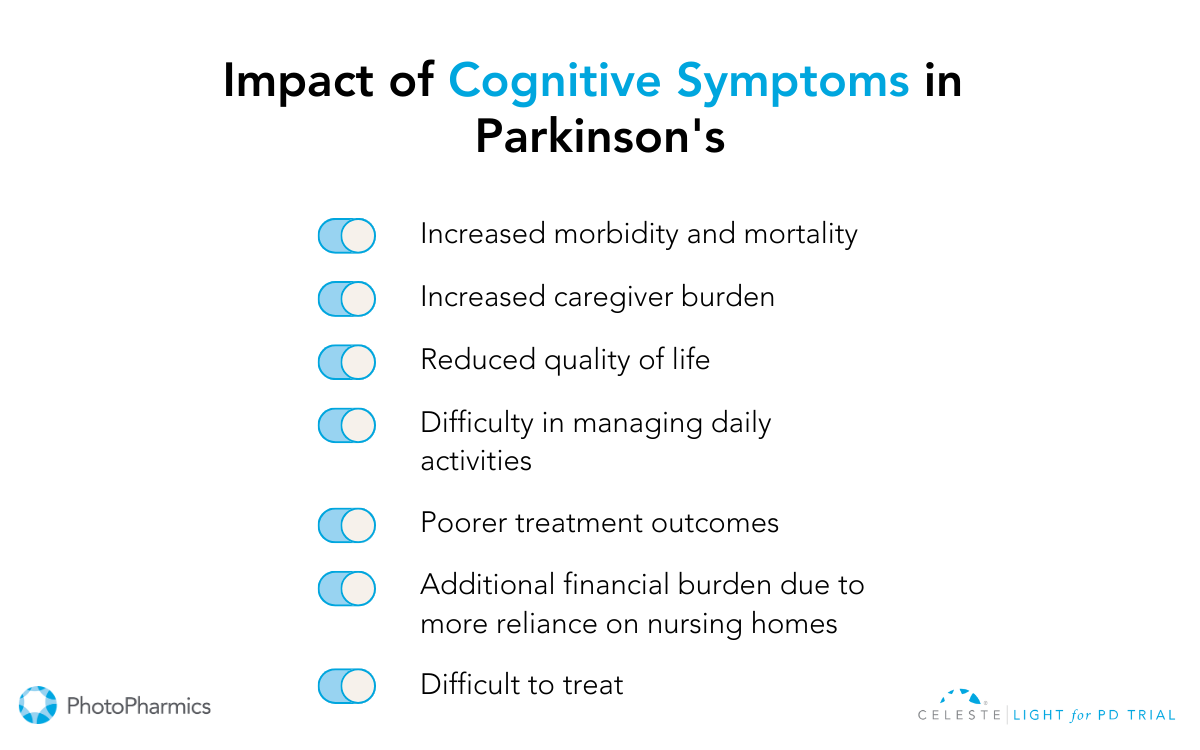
If you’ve ever felt that your mood is a bigger problem than your tremor, you are not alone. Study after study has confirmed that for people with Parkinson’s, depression and anxiety are the single biggest factors that determine a person’s overall quality of life.
It’s not just about feeling sad; these mood states create a vicious cycle of disability that can touch every aspect of your life.
- Worsening Symptoms: Anxiety is known to make tremors worse. Both depression and anxiety are linked to more severe freezing of gait and the difficult “on-off” fluctuations.
- Undermining Self-Care: Depression saps the motivation you need to stick with your medication schedule, do your physical therapy exercises, and stay socially active—all things that are absolutely critical for managing Parkinson’s effectively.
- Accelerating Cognitive Decline: Mood and thinking are deeply connected. Untreated depression can make cognitive issues like problems with focus and attention worse, and over time, may even speed up the rate of cognitive decline.
This ripple effect extends far beyond the individual, placing an enormous strain on the family unit. For caregivers, managing a loved one’s psychiatric symptoms is often more distressing and exhausting than dealing with physical disabilities.
The caregiver’s well-being is directly tied to the patient’s mental state. It’s an incredibly stressful role, and studies show that a huge percentage of caregivers experience burnout and even clinical depression themselves.
Supporting the mental health of the person with Parkinson’s is one of the most important things we can do to support the health of the entire family.
Taking the First Step: Getting the Right Diagnosis
Given the challenge of symptom overlap, you have to be your own best advocate. Don’t wait for your doctor to ask about your mood. In the limited time of a neurology appointment focused on motor symptoms, it can easily be overlooked. You need to start the conversation.
Saying something as simple as, “I’d like to talk about how I’ve been feeling emotionally,” can open the door.
To help identify the problem, your doctor can use simple screening tools. These are short questionnaires that can quickly flag whether you need a more in-depth evaluation.
One of the most recommended for PD is the Geriatric Depression Scale (GDS-15). It’s useful because it focuses more on the psychological feelings of depression and asks fewer questions about physical symptoms that overlap with PD.
The goal of screening isn’t to give a final diagnosis, but to identify that there’s an issue that needs attention. The gold standard is always a full evaluation with a trained mental health professional, like a psychiatrist or neuropsychologist, who can fully understand the nuances of your situation and recommend the best course of action.

Building Your Treatment For Depression and Anxiety in Parkinson’s
Pharmacology is a key part of the treatment plan for many people. It’s about rebalancing the brain chemistry that the disease has disrupted. While no antidepressant is officially FDA-approved specifically for Parkinson’s, several types have been shown to be safe and effective.
Note: This information is for educational purposes only. We do not recommend self-treatment or medication. Please consult a healthcare professional for your Parkinson’s symptoms and receive personalized care options.
Available Options
- SSRIs (Selective Serotonin Reuptake Inhibitors): These are drugs like sertraline (Zoloft) or citalopram (Celexa). They are often the first choice because they are generally well-tolerated. They work by increasing the amount of available serotonin in the brain.
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): These are drugs like venlafaxine (Effexor) or duloxetine (Cymbalta). Because we know that both serotonin and norepinephrine are depleted in PD, these dual-action agents can be a very logical and effective choice.
- TCAs (Tricyclic Antidepressants): An older class of drugs, like nortriptyline, has some of the strongest evidence for effectiveness in PD. However, they come with more side effects (like confusion, dry mouth, and constipation) that can be especially problematic for older adults, so they are usually reserved for cases where other medications haven’t worked.
- Dopaminergic Medications: Sometimes, optimizing your Parkinson’s medication can itself have a positive effect on mood. Certain dopamine agonists (like pramipexole) have been shown to have antidepressant effects. And for anxiety or panic linked to “off” periods, adjusting the timing and dosage of your levodopa is often the most important intervention.
The key is working closely with your doctor. Finding the right medication and the right dose can be a process of trial and error, as suggested or followed by a healthcare specialist.
A thoughtful doctor will practice “symptom-focused prescribing,” choosing a medication that not only helps your mood but whose side-effect profile might help another symptom. For example, if you have depression and insomnia, a more sedating antidepressant might be a great choice.
Non-Medication Strategies For Depression and Anxiety in Parkinson’s
Medication is only one part of the solution. A truly comprehensive plan must include non-pharmacological approaches that empower you with skills and strategies to manage your mental health.
- Cognitive Behavioral Therapy (CBT): CBT is considered a first-line treatment for depression and anxiety in PD. It’s not just “talk therapy.” It is a practical, skills-based approach that teaches you how to identify, challenge, and change the negative thought patterns and behaviors that keep you stuck. For example, it helps you challenge thoughts like “I’m a burden to my family” and work on behavioral activation—scheduling small, achievable, and enjoyable activities to counteract withdrawal and apathy.
- Physical Exercise: Exercise might be a miracle drug for Parkinson’s. A huge body of evidence shows this. Regular activity is a powerful treatment. It’s effective for depression and anxiety. It boosts brain chemicals. It improves sleep. It gives you a sense of control. Find something you enjoy and do it consistently. This can be walking, Tai Chi, or yoga. It can also be a boxing class for PD.
- Social Connection: Isolation is fuel for depression. A lack of social support is one of the biggest risk factors for developing a mood disorder in PD. This is why support groups—either in person or online—can be a lifeline. Connecting with other people who truly “get it” reduces feelings of isolation and provides a space to share experiences and coping strategies.

You’re Not Alone—The Power of an Integrated Care Team in Parkinson’s Depression and Anxiety
Navigating Parkinson’s can feel like trying to coordinate a dozen different specialists who don’t talk to each other. The future of high-quality PD care is moving away from this fragmented system toward an integrated, multidisciplinary team model.
This means having a team of professionals who work together, with you and your family at the center. Your team might include:
- Your Movement Disorder Specialist, who manages the overall disease.
- A Psychiatrist or Psychologist, for medication management and therapy.
- A Clinical Social Worker, to help you connect with community resources.
- Physical, Occupational, and Speech Therapists, whose work to improve your function and independence has a huge positive impact on mood.
In this model, everyone is on the same page, working toward the same goal: improving your overall well-being.
Conclusion
Your emotional well-being is not a “soft” issue. It is not a secondary concern. It is central to your care. The depression and anxiety you feel are real. They are biological. They are treatable.
The first step is to acknowledge the struggle. Start a conversation with your doctor. Talk to your loved ones. Adopt a proactive and multimodal approach. Combine medications with other strategies.
Use therapy, exercise, and social connection. You can effectively manage your mood. Living with Parkinson’s is a journey. It has many challenges. But you don’t have to let this struggle define you. Bring it into the light. This is a crucial step. It helps you live well with Parkinson’s.
A New Ray of Hope: The LIGHT for PD Clinical Trial
For those looking for innovative, non-medication, non-invasive, and at-home approaches, there is promising research underway.
This study is the LIGHT for PD Trial, which is investigating the use of light therapy as a home-based treatment to potentially manage non-motor symptoms of Parkinson’s.
This approach is being explored as a safe, accessible way to potentially improve mood by helping to regulate the body’s internal clock. The trial especially shows promising potential in addressing depression in Parkinson’s.
However, it is close to its end with only 40 last sign-ups left.
So, if you are interested in exploring new treatment options and participating in important research, we encourage you to speak with your doctor or search online for the “LIGHT for PD Clinical Trial” to learn more about the study and see if you might be eligible to participate.
Introduction
Living with Parkinson’s disease presents a unique set of challenges, both physically and emotionally.
While medication plays a crucial role in managing the condition, a holistic approach that incorporates various lifestyle adjustments and self-care strategies can significantly improve your health, well-being, and overall quality of life.
This comprehensive guide explores ten key ways individuals living with Parkinson’s disease can actively manage their symptoms, preserve physical function, and embrace a more fulfilling life.
1. Engage in Regular Physical Activity: Moving Your Body, Empowering Your Life
Research overwhelmingly suggests that regular exercise has a profound positive impact on both the motor and non-motor symptoms of Parkinson’s disease.
Physical activity isn’t just about maintaining mobility; it can actually help prevent or slow the progression of certain symptoms and improve overall strength and brain health.
There are core elements that should be included in a well-rounded exercise regimen for individuals with Parkinson’s:
- Aerobic Exercise: Activities that elevate your heart rate, such as brisk walking, swimming, or cycling, improve cardiovascular health and endurance.
- Strength Training: Exercises like lifting weights or using resistance bands help maintain muscle mass and strength, crucial for daily activities.
- Balance Exercises: Practices such as Tai Chi, yoga, and specific balance drills can significantly improve stability and reduce the risk of falls.
- Stretching and Flexibility: Activities like stretching exercises, yoga, or Pilates help maintain range of motion and reduce muscle stiffness.
The key is to find activities you enjoy and can consistently incorporate into your routine. Start slowly, listen to your body, and always consult with your healthcare professional or a physical therapist before beginning a new exercise program. Noticing how your body responds to different types of movement can also be a subtle way to assess changes in your condition.
Benefits of Exercise for Parkinson’s Patients:
- Maintains and improves mobility and balance.
- Helps manage stiffness and tremors.
- Boosts mood and energy levels.
- Makes everyday tasks easier to accomplish.
- Promotes overall physical and mental well-being.
Tips for Staying Motivated:
- Set small, achievable goals and celebrate your progress.
- Track your activity to visualize your accomplishments.
- Make exercise enjoyable by choosing activities you genuinely like.
- Join a class or exercise with a friend for social support and accountability.

2. Maintain a Balanced Diet: Nourishing Your Body and Mind from Within
A balanced and nutritious diet is an indispensable component of Parkinson’s disease self-care. It provides the essential building blocks for energy, supports muscle and bone health, and positively impacts both physical and mental well-being.
Research even suggests that a healthy diet, rich in fresh vegetables, olive oil, nuts, seeds, and coconut oil, may slow the progression of Parkinson’s disease and ease some symptoms.
Nutritional Needs Specific to Parkinson’s Disease:
- Fiber: Increase intake of fiber-rich foods like whole grains, fruits, vegetables, and legumes to help address constipation, a common symptom.
- Hydration: Drink at least six to eight cups of water or non-caffeinated fluids daily to support digestion and overall bodily functions.
- Calcium and Vitamin D: Ensure adequate intake through low-fat dairy, dark green vegetables, fortified foods, and fatty fish to maintain bone health.
- Protein: Consume healthy protein sources throughout the day, being mindful of potential interactions with certain Parkinson’s medications (discuss timing with your doctor).
- Antioxidants: Include plenty of fruits and vegetables rich in antioxidants to support cellular health.
Foods to Include and Avoid:
- Include: Whole grains, lean proteins, omega-3 fatty acids (found in fatty fish and flaxseeds), and a wide variety of colorful fruits and vegetables.
- Limit: Processed foods, excessive sugar, saturated fats, alcohol, and excessive caffeine. Reduce salt intake to support heart and brain health.
Meal Planning Tips:
- Plan your meals and snacks in advance to ensure you’re consuming nutritious foods.
- Prepare nutrient-dense, easy-to-chew and swallow foods.
- Use simple, manageable recipes to save time and energy.
- Consider keeping a food diary to track your intake and identify any patterns related to your symptoms or medication effectiveness. Pay attention to any digestion changes or unexplained weight loss and consult your doctor if needed.

3. Prioritize Mental Health: Nurturing Emotional Well-being During Parkinson’s
Mental health is a cornerstone of Parkinson’s disease self-care. Managing emotions like stress, anxiety, and depression is crucial for overall well-being and can significantly impact your ability to cope with physical symptoms and daily demands. Prioritizing mental health can improve focus, motivation, and ultimately, your quality of life.
Managing Stress and Anxiety:
- Practice relaxation techniques such as deep breathing exercises, meditation, or mindfulness.
- Establish a structured daily routine to provide a sense of predictability and control.
- Engage in enjoyable activities and hobbies to shift your focus and reduce mental strain.
Techniques for Emotional Well-Being:
- Stay connected with loved ones and express your feelings openly.
- Set achievable goals to foster a sense of accomplishment.
- Consider journaling to process your emotions and track your well-being.
- Engage in light physical activities to boost mood and reduce stress.
Seeking Professional Support:
- Don’t hesitate to reach out to mental health professionals for therapy or counseling if feelings of stress, anxiety, or depression persist.
- Join Parkinson’s disease support groups to connect with others who understand your experiences and share coping strategies.
4. Ensure Adequate Sleep: Restoring Your Body and Mind
Quality sleep is vital for managing energy levels and Parkinson’s disease symptoms. Disrupted sleep can exacerbate motor and non-motor symptoms, making daily activities more challenging. Establishing healthy sleep habits is a crucial aspect of self-care.
Common Sleep Issues in Parkinson’s Patients:
- Insomnia (difficulty falling or staying asleep).
- REM sleep behavior disorder (acting out dreams).
- Restless legs syndrome (uncomfortable sensations in the legs).
- Frequent nighttime awakenings.
Strategies for Improving Sleep Quality During Parkinson’s:
- Maintain a regular sleep schedule, going to bed and waking up around the same time each day.
- Avoid caffeine and alcohol, especially in the evening.
- Create a quiet, dark, and cool sleeping environment.
- Establish a relaxing bedtime routine, such as taking a warm bath, reading, or listening to calming music.
- Engage in gentle stretches or relaxation exercises before bed.
- Limit daytime naps, especially long or late-afternoon naps.
When to Consult a Sleep Specialist:
- Talk to your doctor if sleep problems persist, worsen, or significantly interfere with your daily life. They may recommend a sleep specialist for further evaluation and management.

5. Stay Socially Connected: Nurturing Relationships and Combating Isolation During Parkinson’s
Social interaction plays a powerful role in how individuals cope with Parkinson’s disease. Maintaining connections with friends and family, participating in community activities, or joining hobby groups can significantly reduce feelings of isolation and provide crucial emotional support.
Importance of Social Interaction:
- Provides a sense of connection and belonging.
- Lifts mood and offers fresh perspectives.
- Stimulates attention and memory.
- Strengthens neural networks and improves overall brain health.
Ways to Stay Connected with Friends and Family:
- Schedule regular calls or visits with loved ones.
- Meet for coffee, meals, or shared activities.
- Keep communication open about how you’re feeling and what you need.
Joining Support Groups:
- Connect with others who understand the challenges of living with Parkinson’s disease.
- Share experiences, learn coping strategies, and build a supportive community.
- Your healthcare professional can help you find local support groups, or you can search online resources.

6. Practice Mindfulness and Relaxation Techniques: Cultivating Inner Calm
Managing Parkinson’s isn’t solely about physical health; mental well-being is equally important. Stress and anxiety can often worsen symptoms. Practicing mindfulness and relaxation techniques can help bring a sense of calm, and control, and improve focus, mood, and overall quality of life.
Benefits of Mindfulness for Parkinson’s Patients:
- Helps you stay present in the moment, reducing worry about the future.
- Eases stress and anxiety, which can exacerbate symptoms.
- Improves focus and emotional balance.
- Promotes a greater sense of control over your thoughts and feelings.
Simple Relaxation Exercises:
- Deep Breathing: Inhale slowly through your nose, hold for a few seconds, and exhale slowly through your mouth. Repeat several times.2
- Progressive Muscle Relaxation: Tense and then release each muscle group in your body, starting from your toes and working your way up.3
- Quiet Time: Spend a few minutes each day in a quiet space, focusing on your breath or simply being present.
Incorporating Mindfulness into Daily Routine:
- Start your morning with a few deep breaths.
- Focus on your movements while walking or performing daily tasks.
- Take short breaks throughout the day to notice your surroundings and engage your senses.
7. Manage Medications Effectively: Partnering with Your Healthcare Team
Medications are a vital tool in managing Parkinson’s disease symptoms, helping to maintain motor function and regulate mood. Understanding your medication regimen and adhering to it consistently is crucial for effective symptom control.
Understanding Your Medication Regimen:
- Take the time to learn about each of your medications: what it does, when to take it, and potential side effects.
- Don’t hesitate to ask your doctor or pharmacist any questions you have about your medications.
Tips for Adherence and Managing Side Effects:
- Set reminders or use a pill organizer to help you stay on schedule.
- Pay close attention to any side effects you experience and keep a record of them.
- Communicate any concerns or new symptoms to your doctor; they may be able to adjust dosages or suggest alternative medications.
Communicating with Healthcare Providers:
- Maintain open and honest communication with your neurologist and other healthcare providers.
- Keep them updated on how you’re feeling, any changes in your symptoms, and any challenges you’re facing with your medications.
- Ask questions if anything is unclear; being an active participant in your care is essential.
8. Adapt Your Living Environment: Creating a Safe and Supportive Space
Making modifications to your home environment can significantly enhance safety, comfort, and independence for individuals living with Parkinson’s disease. The goal is to create a space that minimizes the risk of falls and makes daily tasks easier to manage.
Home Modifications for Safety and Comfort:
- Install grab bars in the bathroom near the toilet and shower.
- Add non-slip mats in the bathroom and kitchen.
- Remove loose rugs or clutter from walkways to prevent tripping hazards.
- Ensure good lighting in all rooms and stairways.
- Keep frequently used items within easy reach.
Assistive Devices to Consider:
- Use walking aids such as canes or walkers for added stability.
- Install handrails on stairs.
- Consider a raised toilet seat for easier transfers.
- Explore eating utensils with larger grips or button hooks for dressing if fine motor skills are affected.
- Consult with an occupational therapist for personalized recommendations on assistive devices.
Organizing Daily Activities:
- Establish a daily schedule, prioritizing essential tasks.
- Allow extra time to complete activities without feeling rushed.
- Keep commonly used items in specific, easy-to-remember places.
- Utilize tools like planners or reminders to stay organized and reduce stress.

9. Engage in Cognitive Activities: Keeping Your Mind Sharp and Active During Parkinson’s
Keeping your brain actively engaged is an important aspect of overall well-being for individuals with Parkinson’s disease. Mental stimulation can help maintain focus, memory, and cognitive function, and can also provide a sense of purpose and enjoyment.
Importance of Mental Stimulation:
- Helps slow potential cognitive decline.
- Keeps your mind sharp and engaged.
- Makes it easier to handle daily problem-solving and planning tasks.
- Boosts confidence and provides a sense of accomplishment.
Suggested Cognitive Exercises:
- Try puzzles such as crosswords, Sudoku, or jigsaw puzzles.
- Play memory games or brain-training apps.
- Learn a new skill, such as a language or a musical instrument.
- Read books, articles, or engage in writing.
- Play board games or card games with friends and family.
- Engage in hobbies that challenge your thinking.
Incorporating Cognitive Activities into Daily Life:
- Dedicate specific time slots for cognitive exercises.
- Integrate mental stimulation into your daily routine, such as reading during breaks or solving a puzzle with your morning coffee.
- Engage in conversations that challenge your thinking and expand your knowledge.

10. Explore Complementary Therapies: Integrating Holistic Approaches
In addition to traditional medical treatments and lifestyle adjustments, many individuals with Parkinson’s disease find benefit in exploring complementary therapies. These approaches, used alongside conventional care, can help manage specific symptoms, promote relaxation, and enhance overall well-being.
Overview of Complementary Therapies:
- Yoga: Can improve flexibility, balance, strength, and potentially mood and sleep. Adapted yoga classes for movement disorders are particularly beneficial.
- Tai Chi: Promotes balance, coordination, and stability, showing measurable improvements in individuals with moderate Parkinson’s.
- Massage Therapy: May provide temporary relief from muscle rigidity and resting tremor, and can also induce relaxation and improve sleep.
- Movement Therapies (e.g., Alexander Technique, Feldenkrais Method): Focus on posture, balance, and retraining the body for easier movement, potentially helping maintain mobility.
- Acupuncture: Some individuals report relief from fatigue and poor sleep with acupuncture, although human studies on neuroprotective effects are still limited.
- Nutritional Supplements: While some supplements like Co-Q10 haven’t shown consistent benefits in studies, calcium supplementation may be important due to dietary adjustments related to medication absorption. Always consult your doctor before starting any new supplement and never stop taking your prescribed medications.
Evaluating the Benefits and Risks:
- Discuss any complementary therapies you are considering with your doctor to ensure they are safe and appropriate for your individual situation.
- Research practitioners and methods to ensure they are reputable and evidence-based where possible.
- Keep track of how you feel after trying a new therapy to determine if it is providing any benefit.
Integrating Therapies into Your Care Plan:
- Complementary therapies should be viewed as an adjunct to your regular healthcare plan, not a replacement.
- Openly discuss your interest in these therapies with your healthcare provider to ensure a coordinated and safe approach to your care.

Conclusion: Embracing a Proactive Approach to Living Well with Parkinson’s Disease
Managing Parkinson’s disease effectively involves a multifaceted approach that extends beyond medication.
By actively incorporating regular exercise, a balanced diet, mental health strategies, quality sleep habits, social engagement, mindfulness, effective medication management, environmental adaptations, cognitive stimulation, and exploring complementary therapies, individuals living with Parkinson’s can take a proactive role in managing their symptoms, maintaining their independence, and enhancing their overall quality of life.
Remember that self-care is not a luxury but a necessity in navigating the challenges of Parkinson’s disease and embracing a dignified and fulfilling life.
Join the Light in the Fight Against Parkinson’s

Living with Parkinson’s Disease (PD) can be challenging. While medications and surgeries offer some relief, many individuals still face significant non-motor symptoms.
PhotoPharmics is pioneering a non-invasive approach to address these challenges. Our Light for PD clinical trial is seeking participants to evaluate the effectiveness of the Celeste therapeutic light device.
This six-month, at-home study is designed for people aged 45 and older with a Parkinson’s diagnosis and offers up to $500 for full participation.
By joining this clinical trial, you could help revolutionize care while exploring a therapy that might enhance your own well-being.
Check your eligibility today—let’s brighten the future together!
Introduction
“My father experienced hallucinations and delusions, and at the time, we didn’t realize these symptoms were part of his Parkinson’s disease. My mom tried to shield my family and carry the burden alone each day. I wish l’d known there was more to Parkinson’s than motor symptoms, which is why l’m encouraging people and families affected by Parkinson’s to talk early and often about hallucinations and delusions.”
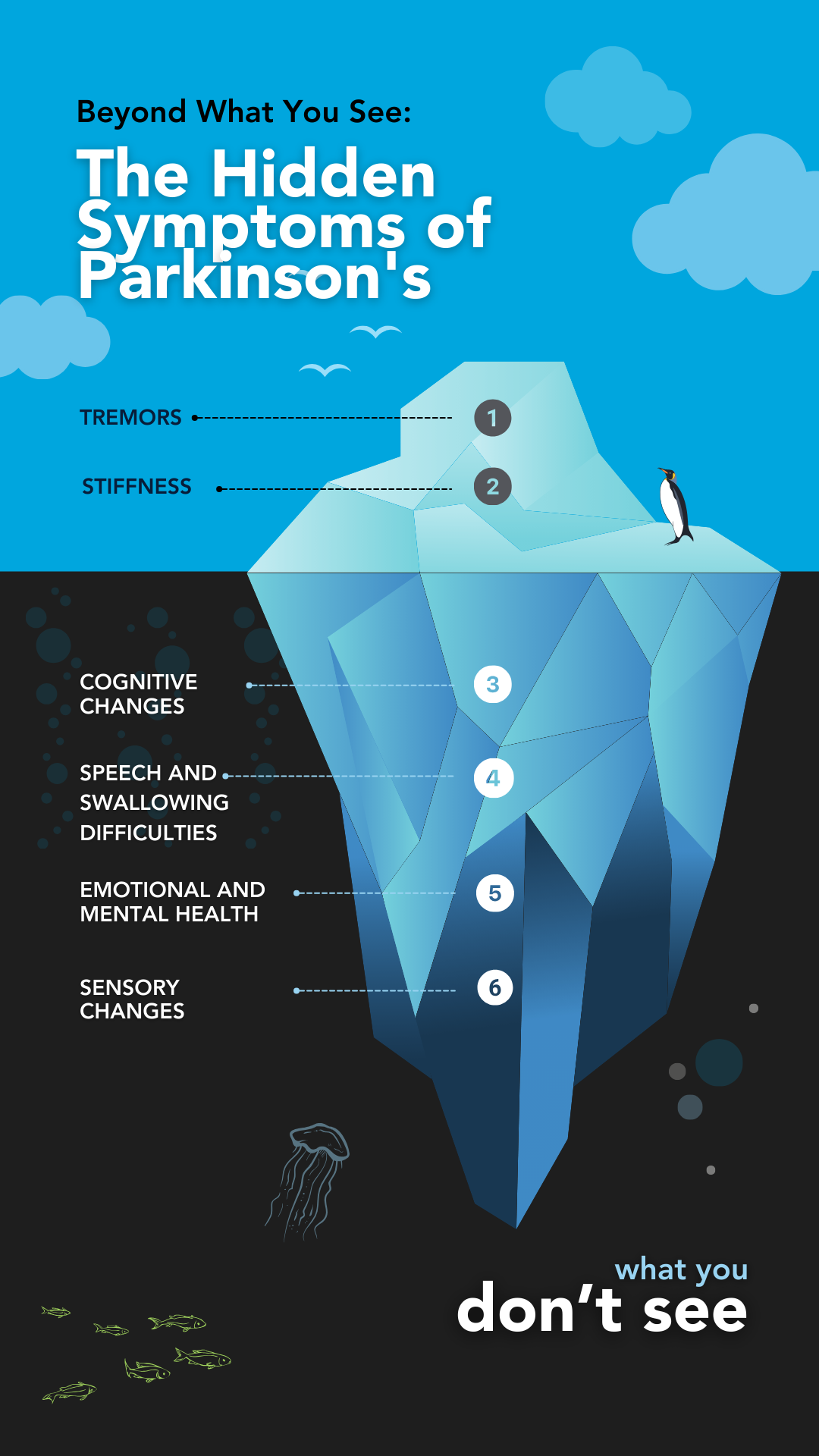
This heartfelt reflection by actor and advocate Ryan Reynolds highlights an often-overlooked reality: Parkinson’s disease is far more than tremors and motor issues.
While most of us recognize Parkinson’s disease for its visible motor symptoms, these are merely “the tip of the PD iceberg.”
Beneath the surface lies a host of non-motor symptoms—such as hallucinations, delusions, sleep disturbances, anxiety, and cognitive changes—that can profoundly affect the quality of life for both patients and their caregivers.
In this article, we’ll dive deeper into the non-motor aspects of Parkinson’s disease, learn why they occur, and provide practical insights for managing these symptoms effectively.
Understanding the full picture of Parkinson’s is key to fostering better care, awareness, and support for those affected.
What are The Non-Motor Symptoms of Parkinson’s?
Parkinson’s disease (PD) is often recognized for its motor symptoms, such as tremors and stiffness. However, an equally significant aspect of PD is its non-motor symptoms, which can profoundly impact daily life.
These symptoms can precede motor signs by years, making early identification crucial.
Here’s a breakdown of the common non-motor symptoms, what they entail, why they occur, and their impact:
Cognitive and Emotional Challenges
- Cognitive Impairment: Issues like memory loss, slower thinking (bradyphrenia), and difficulty multitasking occur as Parkinson’s affects brain regions controlling cognition. Over time, this can progress to mild cognitive impairment or dementia.
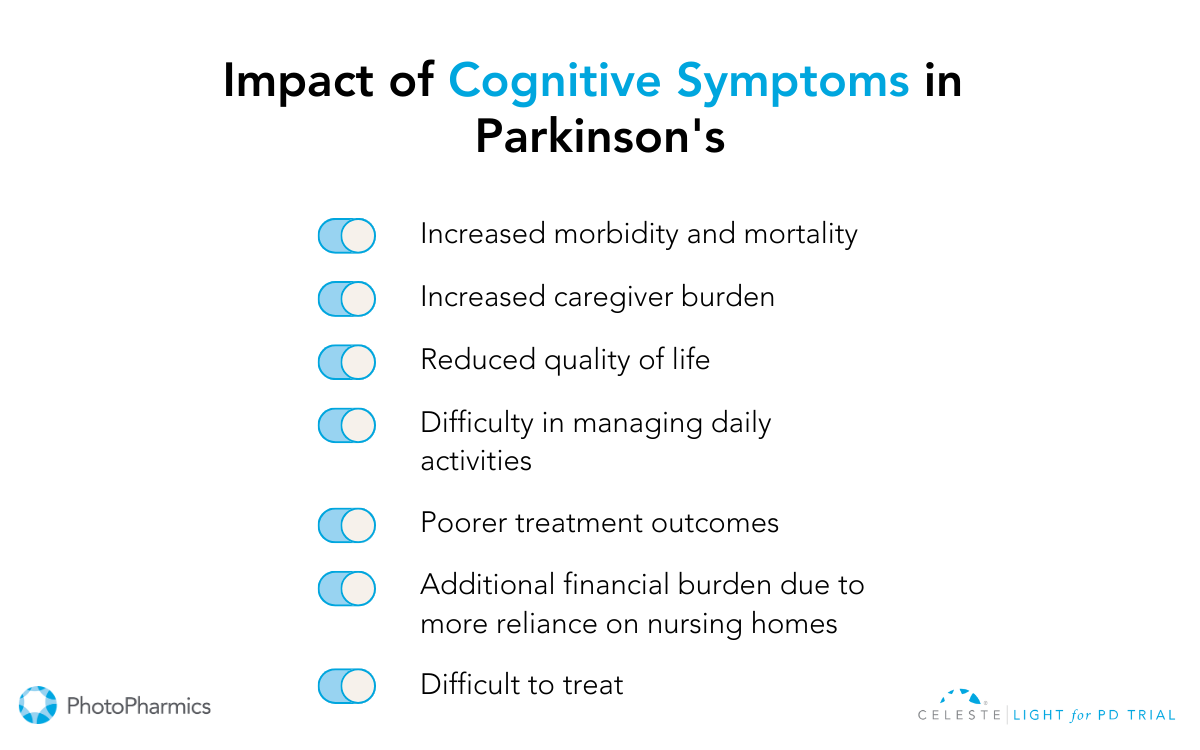
- Depression and Anxiety: Changes in brain chemistry, particularly dopamine levels, can trigger mood disorders. These conditions often begin early and can significantly affect quality of life.
- Hallucinations and Delusions: Hallucinations involve seeing or hearing things that aren’t there, while delusions are false beliefs. These symptoms are often associated with long-term use of Parkinson’s medications or disease progression.
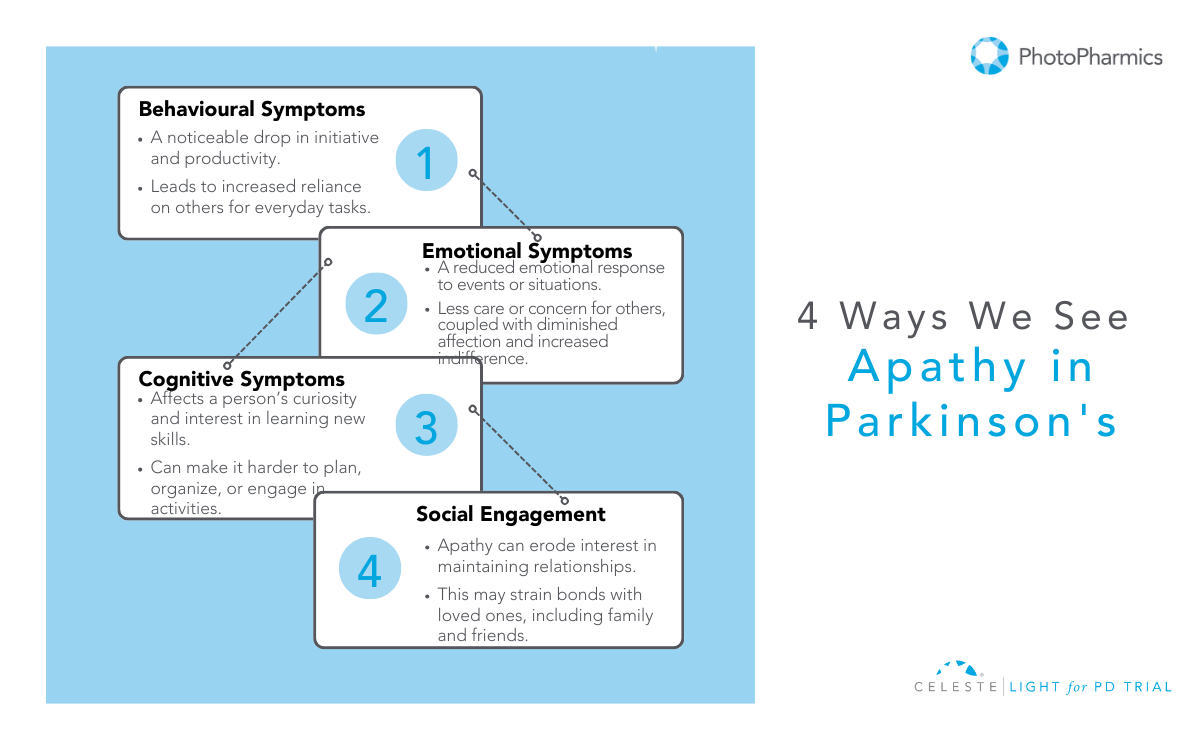
- Apathy: A lack of motivation that may be mistaken for intentional behavior but stems from neurological changes. It can significantly impact not only the person living with PD but also their loved ones. Apathy manifests in three ways:
— Cognitive: Reduced curiosity or interest in new things.
— Emotional: A lack of passion or reaction to events or news that would normally spark emotions.
— Behavioral: Difficulty starting activities and needing prompts to complete tasks.
Sensory and Autonomic Symptoms
- Skin and Sweating: Excessive sweating or oily skin is common due to overactive sweat glands. Dry skin can also occur in some individuals.
- Loss of Smell: Often one of the first signs of Parkinson’s, this is linked to early degeneration of specific brain cells.
- Pain and Tingling: Nerve dysfunction or rigidity can cause discomfort in various parts of the body.
- Rigidity: Stiffness throughout the body or in specific areas can lead to discomfort and restricted movement, often mistaken for normal aging.
- Autonomic Dysfunctions:
- Constipation: Impaired digestion due to slowed gut movement.
- Urinary Issues: A frequent need to urinate or incontinence caused by bladder muscle dysfunction.
- Lightheadedness: Sudden drops in blood pressure when standing (orthostatic hypotension).
- Sweating and Salivation: Overactive glands leading to excessive sweating or drooling.
Speech and Communication Issues
- Speech Problems: Many individuals experience reduced voice volume (hypophonia), monotone speech, or difficulty articulating words. This results from the reduced coordination of muscles involved in speaking.
Fatigue and Sleep Problems
- Chronic Fatigue: Often caused by disrupted sleep cycles, low dopamine levels, or medication side effects.
- Sleep Disturbances: These include difficulty falling asleep, vivid dreams, or REM sleep behavior disorder.
How To Manage Non-Motor Symptoms of Parkinson’s?
While it’s true that Parkinson’s disease currently has no cure, it doesn’t mean its progression cannot be delayed or its symptoms managed.
What does this mean?
Although you cannot eliminate Parkinson’s, you can slow down its progression and reduce its impact on your physical and mental health. This can be achieved by adopting certain lifestyle changes, such as maintaining a healthy diet, staying physically active, managing stress, and ensuring good sleep hygiene or taking targeted treatments.
Taking proactive steps can help you improve your quality of life and empower you to manage your condition better.

Cognitive and Emotional Challenges
Managing cognitive and emotional challenges in Parkinson’s Disease (PD) involves a multi-faceted approach that combines professional therapies and everyday strategies to enhance mental well-being and daily functionality.
Treatment Options and Tips:
-
Cognitive Remediation Therapy
This therapy focuses on teaching individuals alternative ways to manage memory or thinking problems by leveraging their cognitive strengths. It is particularly effective for those with mild cognitive deficits. Neuropsychologists or speech-language pathologists often conduct these sessions in a supportive environment, helping both individuals and caregivers apply practical strategies for daily tasks. While it doesn’t reverse cognitive challenges, it equips individuals with tools to improve their quality of life.
Simple environmental changes can reduce cognitive stress and confusion. Decluttering living spaces minimizes distractions while using nightlights can prevent disorientation during nighttime. Establishing a structured daily routine provides clarity and stability, which can help manage issues like impulsivity and difficulties with communication.
By incorporating these treatments and strategies, individuals with Parkinson’s and their caregivers can navigate cognitive and emotional hurdles more effectively, fostering a sense of control and improving overall quality of life.
Sensory and Autonomic Symptoms
- Sweating: Excessive sweating can be managed by adjusting carbidopa-levodopa doses under medical guidance. Lukewarm showers, lightweight clothing, and staying hydrated are practical tips to reduce discomfort, while severe cases may benefit from prescribed medications.
- Skin Issues: For dry or flaky skin, washing with warm water, using unscented glycerin soap, and applying moisturizers can help. Persistent issues like dandruff may require medicated shampoos or dermatological advice.
- Loss of Smell: No specific treatment is available, but monitoring dietary intake can help if appetite changes. Focus on balanced nutrition and seek guidance on maintaining a healthy weight if smell impacts eating habits.
- Pain and Tingling: To reduce stiffness, address nerve dysfunction through tailored exercises, such as stretching or yoga. Speak to your doctor about medications or therapies to effectively manage chronic pain. According to the Parkinson’s Foundation, some therapies used to manage the condition include Deep Brain stimulation (DBS), Botulinum Injections (Botox®), and surgery.
- Autonomic Dysfunctions:
- Constipation: To manage constipation effectively, incorporate a diet rich in fiber, including plenty of fruits, vegetables, and whole grains. Staying hydrated is equally important—aim to drink 48 to 64 ounces of water daily, and consider warm liquids in the morning to help stimulate digestion. Regular physical activity can further support healthy bowel function. If these measures aren’t sufficient, consult your doctor about adding fiber supplements or stool softeners to your routine.
- Urinary Issues: Monitor fluid intake to avoid overhydration while managing urgency. Discuss bladder training or medications with your doctor for better control.
- Lightheadedness: Stand up slowly to prevent sudden drops in blood pressure. Increase salt and water intake under medical supervision and wear compression stockings if advised by your doctor.

Speech and Swallowing Issues
Speech and swallowing challenges in Parkinson’s disease can be effectively managed through targeted therapies.
Managing Speech Issues
Speech-language pathologists (SLPs) play a critical role by tailoring exercises to improve vocal strength, clarity, and swallowing function. Evidence-based programs such as Lee Silverman Voice Treatment (LSVT) and Parkinson Voice Project SPEAK OUT! offer specialized support. For additional aid, assistive devices like voice amplifiers and exercises for articulation, posture, and breathing can enhance communication.
Further, maintaining hydration, practicing daily vocal exercises, and reducing background noise are key strategies to manage speech problems. Scheduling speech therapy early can help prevent worsening symptoms, and communication tools can support interactions.
Managing Swallowing Issues
Swallowing difficulties often benefit from dietary adjustments, such as softer food textures or thicker liquids, and exercises like expiratory muscle strength training, guided by an SLP.
Additionally, consulting an SLP for evaluation and following their recommendations, including modified diets and muscle training, ensures safer and more efficient eating to manage swallowing problems. Regular follow-ups and tailored interventions help improve quality of life.

Fatigue and Sleep Problems
Sleep challenges in Parkinson’s disease can often be managed with a combination of lifestyle changes, therapy, and medication.
- Maintaining a consistent sleep schedule, creating a calming bedtime routine, and ensuring a cool, dark sleeping environment can improve sleep quality.
- Daily outdoor activity and morning exercise help regulate the sleep-wake cycle, while light therapy can assist those unable to get outdoors.
- Limiting screen time and stimulating substances like caffeine before bed, as well as reducing fluid intake in the evening, can also minimize nighttime disruptions.
- For turning difficulties, satin sheets and pajamas or lightweight quilts are recommended.
Medical interventions can address specific issues like urinary frequency or medication side effects affecting sleep.
Doctors may prescribe medications such as oxybutynin or tolterodine for bladder-related disturbances (according to Parkinson’s Foundation), or antidepressants like mirtazapine for sleep support, though individual responses vary.
Consulting a sleep specialist or urologist for tailored treatments is advised. Avoiding anxiety-inducing activities and late-night heavy meals further supports restful sleep, ensuring better management of PD-related sleep concerns.
Be Part of the Light Against Parkinson’s: Participate in the Light for PD Clinical Trial

Managing Parkinson’s disease (PD) can be overwhelming, with many individuals experiencing persistent non-motor symptoms even after medications or surgeries.
PhotoPharmics is at the forefront of exploring innovative, non-invasive therapies to address these challenges. Our Light for PD clinical trial focuses on evaluating the Celeste therapeutic light device, designed to offer new hope for those living with PD.
This six-month, home-based study welcomes participants aged 45 and older with a Parkinson’s diagnosis and provides up to $500 for full participation.
By joining, you’ll contribute to groundbreaking research that could transform PD care while discovering a therapy with the potential to enhance your quality of life.
Check your eligibility today—let’s illuminate a brighter future together!
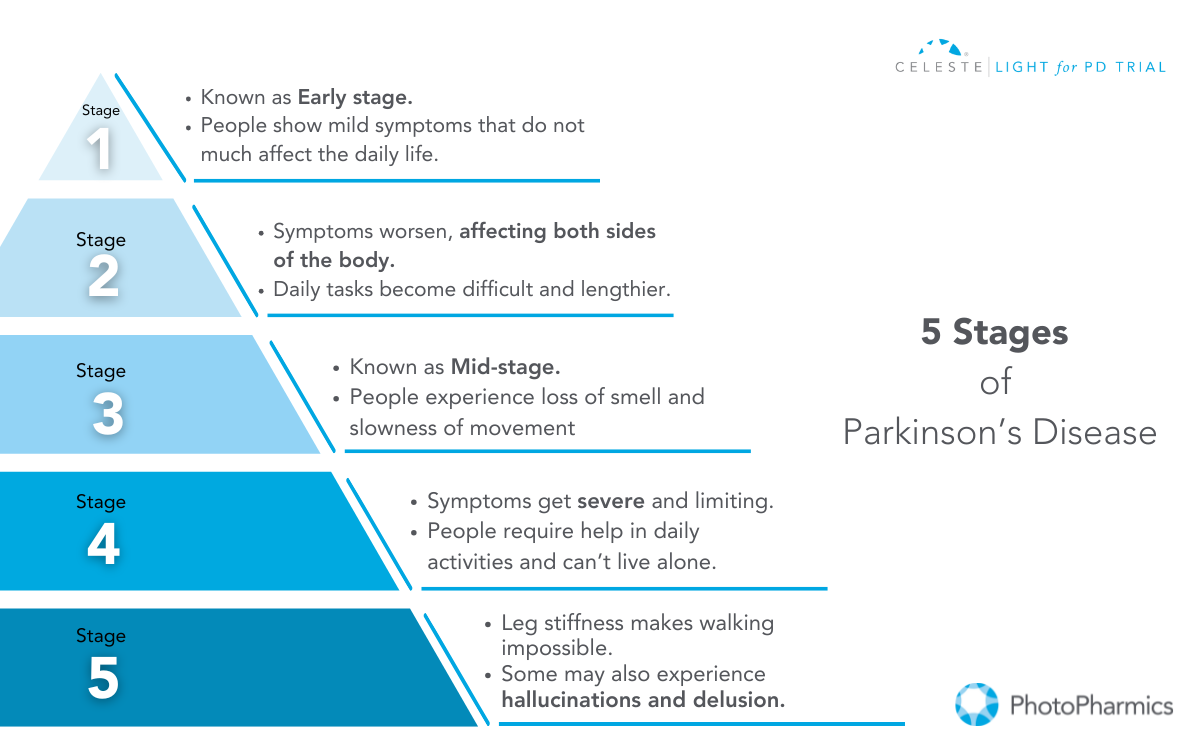
What is Parkinson’s?
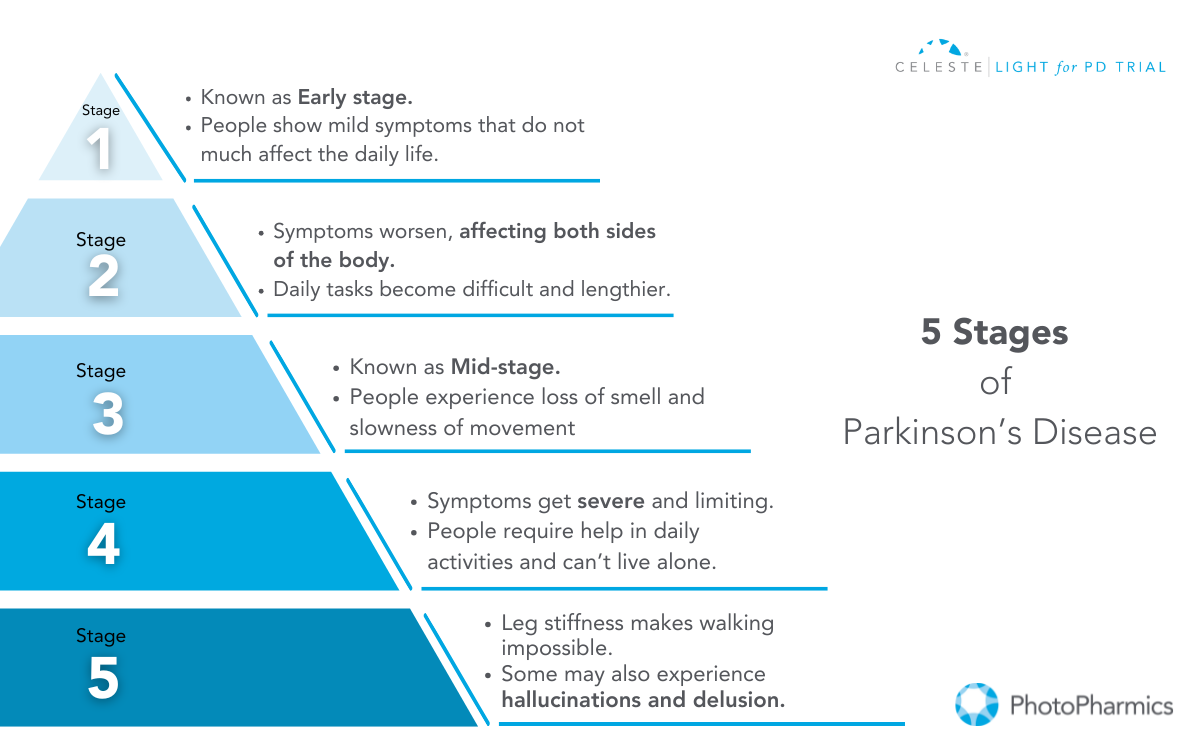
Parkinson’s Disease (PD) is a complex neurodegenerative disorder that affects the nervous system and progressively worsens over time.
While motor symptoms—such as tremors, stiffness, and slow movement—are often the most observable and commonly associated with the condition, Parkinson’s encompasses a broader spectrum of challenges.
Non-motor symptoms (NMS), including anxiety, depression, apathy, and sleep disturbances, can occur early in the disease’s course, sometimes even before motor symptoms appear. Together, these symptoms profoundly impact the daily lives of those with Parkinson’s.
Currently, there is no cure available to treat the disease; however, medicines, therapies, and certain lifestyle changes may help you manage and slow the progression of Parkinson’s symptoms.
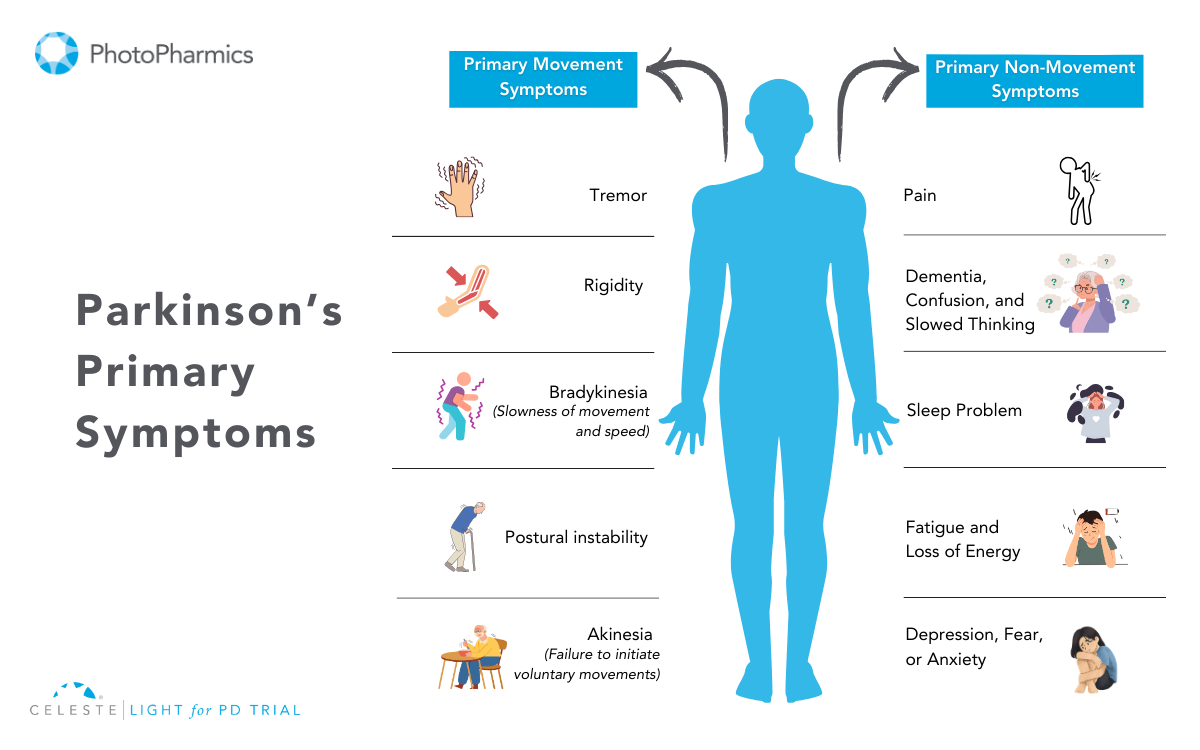
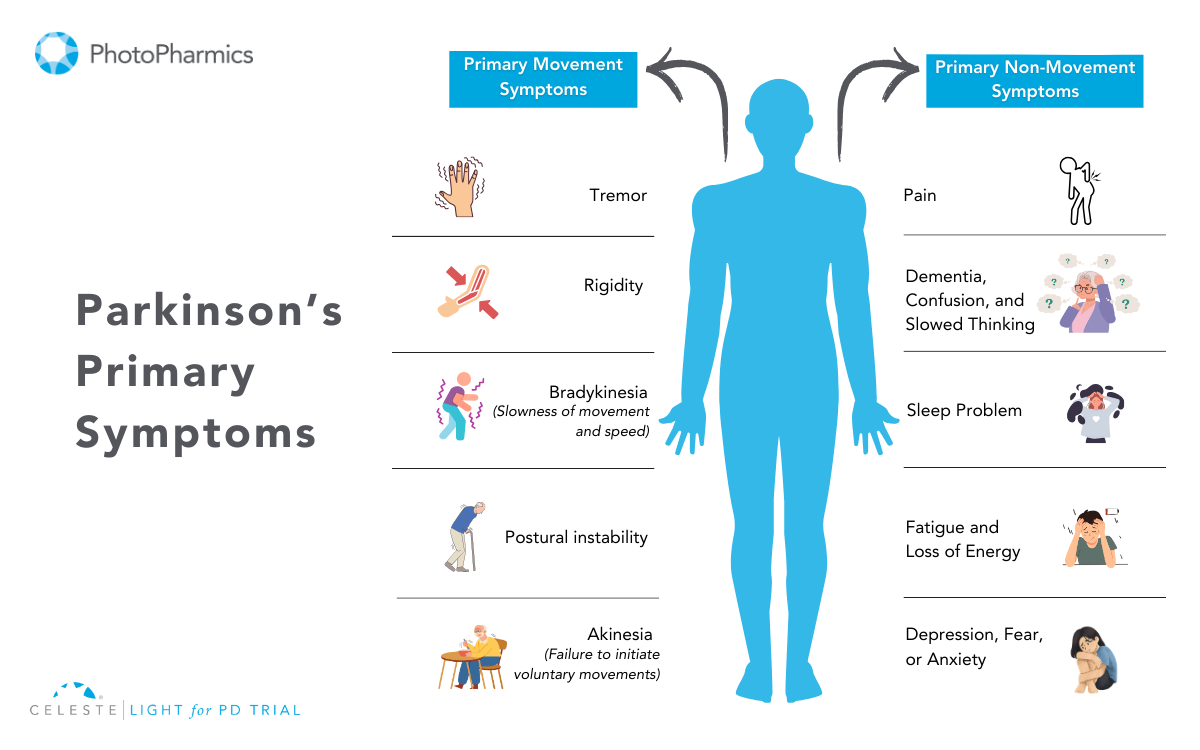
Symptoms of Parkinson’s Disease
Parkinson’s symptoms are typically categorized into two types: motor (movement) and non-motor (non-movement) symptoms. Both play significant roles in shaping the overall experience of living with PD.
Motor Symptoms
Motor symptoms arise from the brain’s reduced ability to regulate movement due to the loss of dopamine-producing cells. These symptoms can vary in severity but often have a significant impact on daily life.
Here’s an overview of key motor symptoms:
- Tremor: Tremor is one of the hallmark symptoms of PD, typically beginning in the hands or fingers and occasionally affecting the foot or jaw. It is most noticeable when the person is at rest or under stress. A common sign is the “pill-rolling” motion, where the thumb and forefinger rub together rhythmically. Interestingly, the tremor usually subsides during sleep or purposeful movements.
- Slowed Movement: Bradykinesia, or the slowing of spontaneous movement, can make routine tasks like dressing, showering, or eating much harder. Activities that were once quick and effortless may become prolonged and laborious. Additionally, facial expressions might diminish, leading to a “masked face” appearance.
- Balance or Posture Problems: Postural instability and balance issues are common in PD, leading to a stooped posture and a higher risk of falls. Individuals may develop a distinctive “Parkinsonian gait,” characterized by quick, shuffling steps (festination) and reduced arm swing. Freezing of movement, where a person temporarily feels stuck in place, can also occur.
- Small Hand-Writing: Micrographia, or abnormally small handwriting, often becomes evident in individuals with PD. Letters may appear cramped and harder to read, reflecting the motor difficulties associated with fine hand movements.
- Muscle Stiffness or Rigidity: Rigidity affects most people with PD, causing muscles to remain tense and resistant to movement. This can lead to discomfort, aches, and reduced range of motion. When another person attempts to move the arm or leg, it may move in short, jerky motions, often referred to as “cogwheel rigidity.”
Non-Motor Symptoms
Non-motor symptoms often emerge early, sometimes years before motor symptoms, and significantly impact emotional, mental, and physical well-being.
The non-motor symptoms of Parkinson’s include:
- Mental Health Issues (Anxiety/Depression): Parkinson’s affects more than just movement; it also deeply influences mental well-being. Many individuals experience anxiety and depression. Anxiety manifests as uncontrollable worry, while depression can lead to sadness, loss of energy, and decreased interest in daily activities. These mood disturbances are not just a response to the diagnosis but a part of the disease itself, rooted in changes within the brain.
- Digestion Problem: Constipation and other digestive issues are common due to the slowing of the digestive tract caused by Parkinson’s. This can make it harder for individuals to maintain proper nutrition and can lead to discomfort if not managed effectively.
- Sleep Problem: Sleep disturbances, such as trouble falling asleep, restless nights, or excessive daytime sleepiness, are prevalent in Parkinson’s. Conditions like REM sleep behavior disorder (acting out dreams) can disrupt rest and pose safety risks. Some sleep issues may be linked to medications or the disease itself.
- Loss of Smell: Loss of smell is one of the earliest signs of Parkinson’s, often occurring years before motor symptoms. This can affect appetite, as the sense of smell is closely tied to taste and enjoyment of food.
- Urinary Issues: Parkinson’s can disrupt autonomic functions, leading to frequent urination, incontinence, or difficulty emptying the bladder. Constipation is also common due to slowed digestive processes. These issues can significantly affect daily life and require tailored management strategies.
- Speech Problem: Changes in speech, such as a soft or monotone voice, are often noted in people with PD. Some may experience difficulty articulating words clearly or find it challenging to speak at an appropriate volume, which can make communication harder.
- Cognitive Issues: Parkinson’s disease can significantly impact emotional well-being and cognitive function. Apathy, or a lack of motivation, is common and may affect daily activities. Cognitive issues range from mild difficulties, like trouble concentrating, to more severe problems, such as dementia. These changes can interfere with social interactions, work, and overall quality of life, making early intervention and management crucial.
- Swallowing or chewing problem: In the later stages of Parkinson’s, swallowing and chewing can become challenging due to weakened muscle control. Food or saliva may accumulate in the throat, increasing the risk of choking or drooling. These difficulties can lead to nutritional deficiencies, necessitating dietary modifications or medical intervention.
Both motor and non-motor symptoms are critical to understanding Parkinson’s as a whole, as they collectively shape the experience of those living with the condition. Recognizing and addressing both types is essential for effective management.
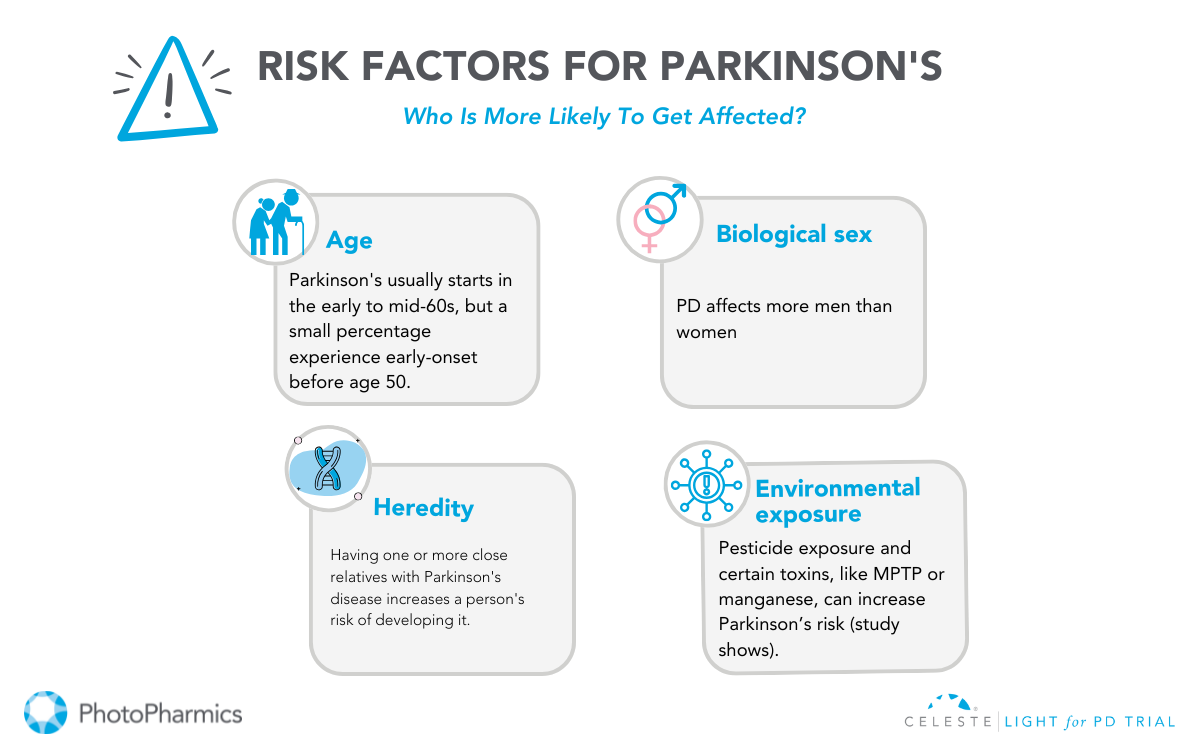
What Causes Parkinson’s?
The exact cause of Parkinson’s remains unknown, but it is believed to result from a combination of genetic, environmental, and lifestyle factors.
1. Genetic Factors
Genetic mutations contribute to 10-15% of Parkinson’s cases. Specific gene variations, like LRRK2 or SNCA, are linked to a higher risk, but most cases are not directly caused by a single mutation. Genetic research continues to explore these connections for better prevention and treatment strategies.
2. Environmental Exposures
Exposure to pesticides, traumatic head injuries, or certain toxins has been associated with increased PD risk. However, many people with such exposures do not develop Parkinson’s, suggesting other contributing factors are involved.
3. Aging
Aging is the most significant risk factor. Most diagnoses occur after age 60, though early-onset Parkinson’s can appear in younger individuals.
4. Brain Changes
The disease involves the loss of dopamine-producing neurons in the substantia nigra, a brain area crucial for movement control. This neuronal loss leads to Parkinson’s symptoms.
PD arises from a complex interplay of factors, and ongoing research is vital to understanding its causes and progression.
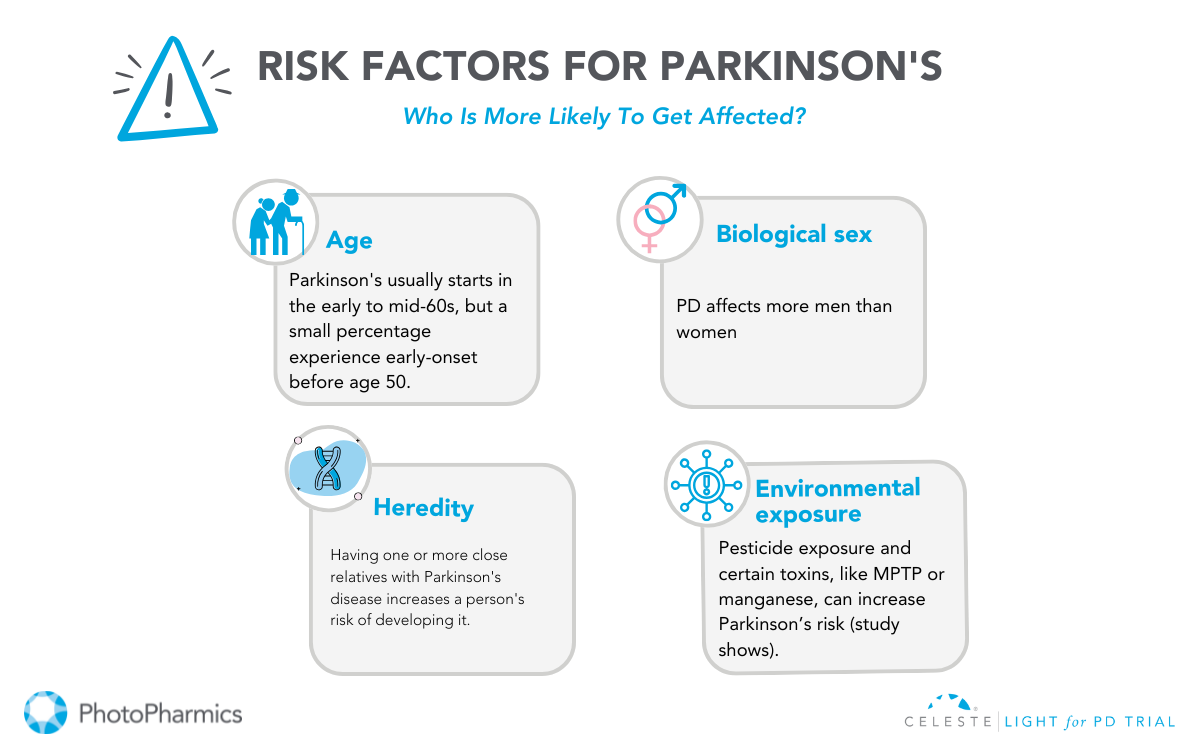
Who Can Get Parkinson’s?
Parkinson’s disease, a progressive neurological disorder, predominantly affects older adults. While the exact cause remains elusive, certain factors can elevate the risk of developing this condition.
Age and gender play significant roles, with the risk increasing with age and men being more susceptible. Environmental factors, such as long-term exposure to pesticides and heavy metals, can also contribute to the risk.
Additionally, genetic factors, particularly a family history of Parkinson’s and specific gene mutations, can increase susceptibility.
Other risk factors include REM sleep behavior disorder and traumatic brain injury. It’s crucial to note that while these factors can influence the risk, not everyone with these factors will develop Parkinson’s.
Diagnosis and Treatment of Parkinson’s
While there’s no cure for Parkinson’s, understanding the diagnostic process and treatment options is crucial for managing the condition effectively.
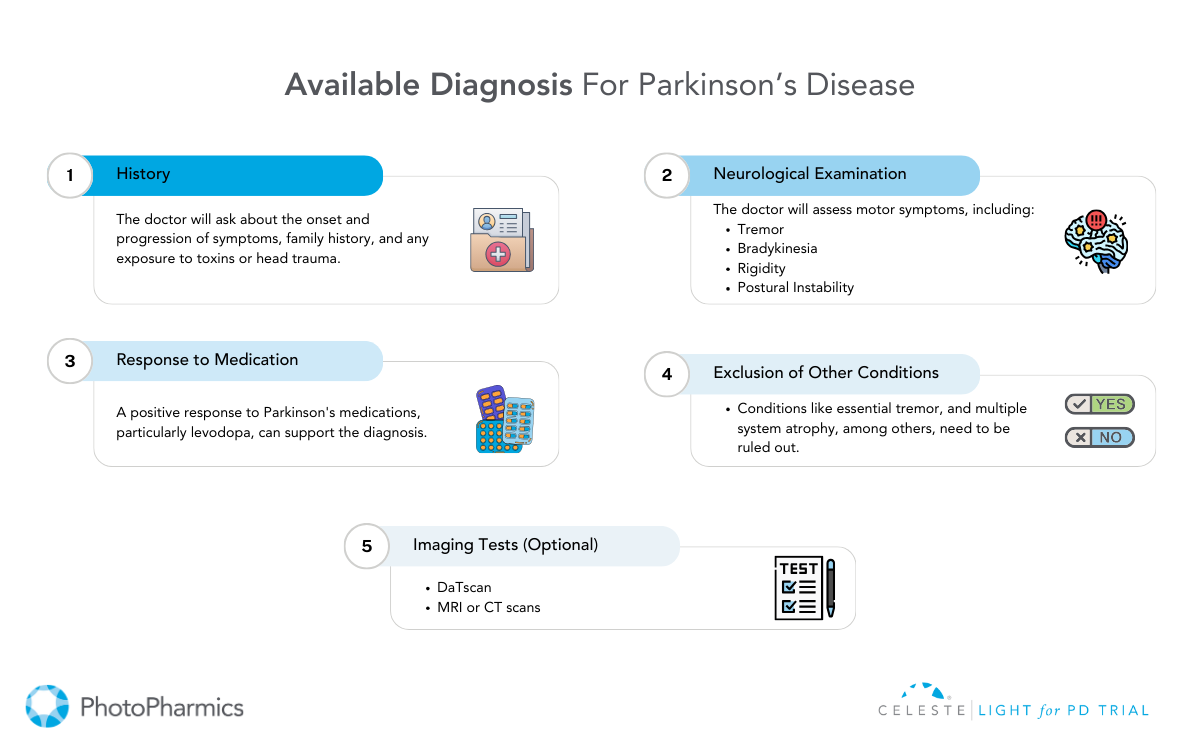
Diagnosis of Parkinson’s Disease
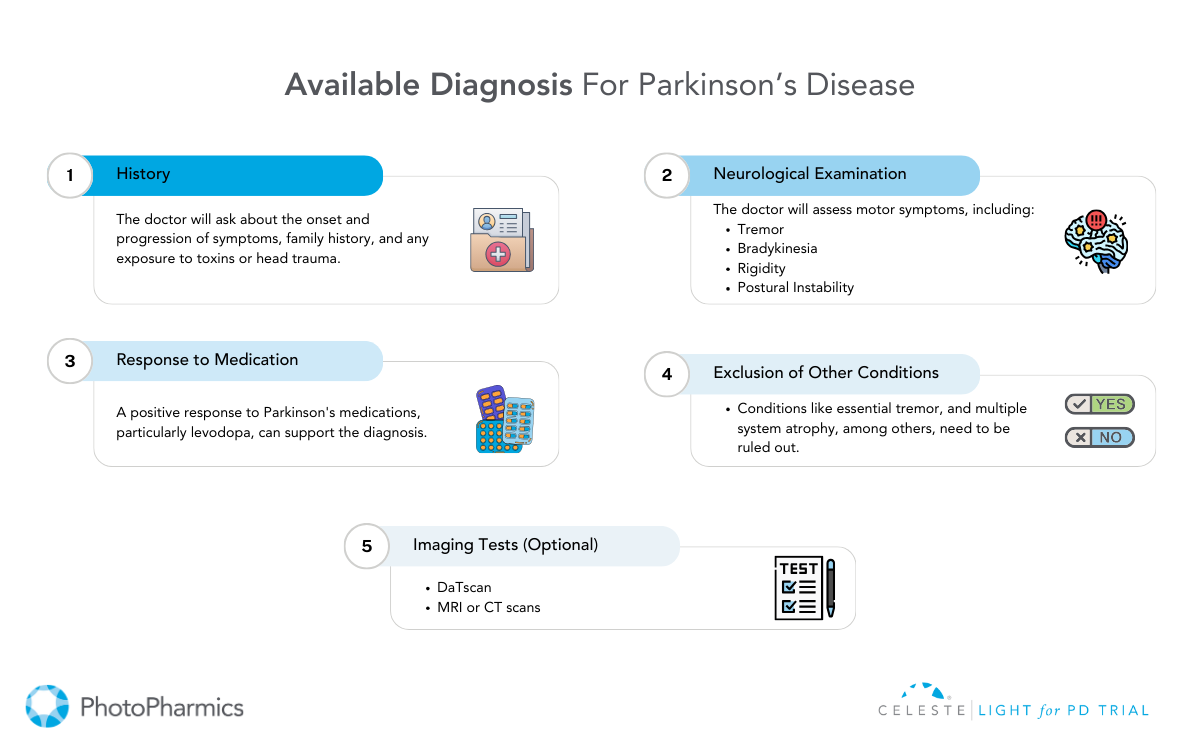
Diagnosing Parkinson’s Disease (PD) involves a comprehensive evaluation by a neurologist. There’s no single definitive test, but a combination of methods helps identify the characteristic symptoms.
The neurologist reviews the patient’s medical history, conducts a neurological examination to assess motor skills and cognitive function, and may order specialized tests.
Brain imaging techniques like MRI and DaTscan can provide valuable insights into brain structure and function. A careful evaluation of how symptoms respond to medications like levodopa can also aid in diagnosis.
Treatment of Parkinson’s Disease
While there’s no cure for Parkinson’s Disease, various treatment options can help manage symptoms and improve quality of life.
Medication plays a crucial role, with dopamine replacement therapy being the cornerstone. Medications like levodopa increase dopamine levels in the brain, while other drugs mimic its effects or slow its breakdown.
In addition to medication, surgical interventions like deep brain stimulation (DBS) and focused ultrasound (FUS) may be considered for specific cases.
Non-pharmacological therapies, including physical therapy, occupational therapy, and speech therapy, complement medical treatments by addressing mobility, daily living activities, and communication challenges.
The journey with Parkinson’s may be challenging, but with a strong support system and the right healthcare provider, you can navigate it more effectively.
Surround yourself with loved ones who can provide emotional and practical support, and explore the wealth of resources available to help make living with Parkinson’s easier and more manageable.
Join the Light in the Fight Against Parkinson’s

Living with Parkinson’s Disease (PD) can be challenging. While medications and surgeries offer some relief, many individuals still face significant non-motor symptoms.
PhotoPharmics is pioneering a non-invasive approach to address these challenges. Our Light for PD clinical trial is seeking participants to evaluate the effectiveness of the Celeste therapeutic light device.
This six-month, at-home study is designed for people aged 45 and older with a Parkinson’s diagnosis and offers up to $500 for full participation.
By joining this clinical trial, you could help revolutionize care while exploring a therapy that might enhance your own well-being.
Check your eligibility today—let’s brighten the future together!