Introduction
Welcome back to our exploration of groundbreaking advancements in Parkinson’s Disease (PD) treatment.
In Part 1, we dived into the potential of light therapy, other innovative non-pharmacological approaches like Focused Ultrasound and Transcranial Magnetic Stimulation, novel rehabilitation strategies, and the evolving landscape of drug candidates targeting core PD pathologies like alpha-synuclein, neuroinflammation, and specific genetic links.
Now, we turn our attention to even more revolutionary frontiers: biological game-changers like gene and stem cell therapies, and the incredible impact of technology in reshaping Parkinson’s care.
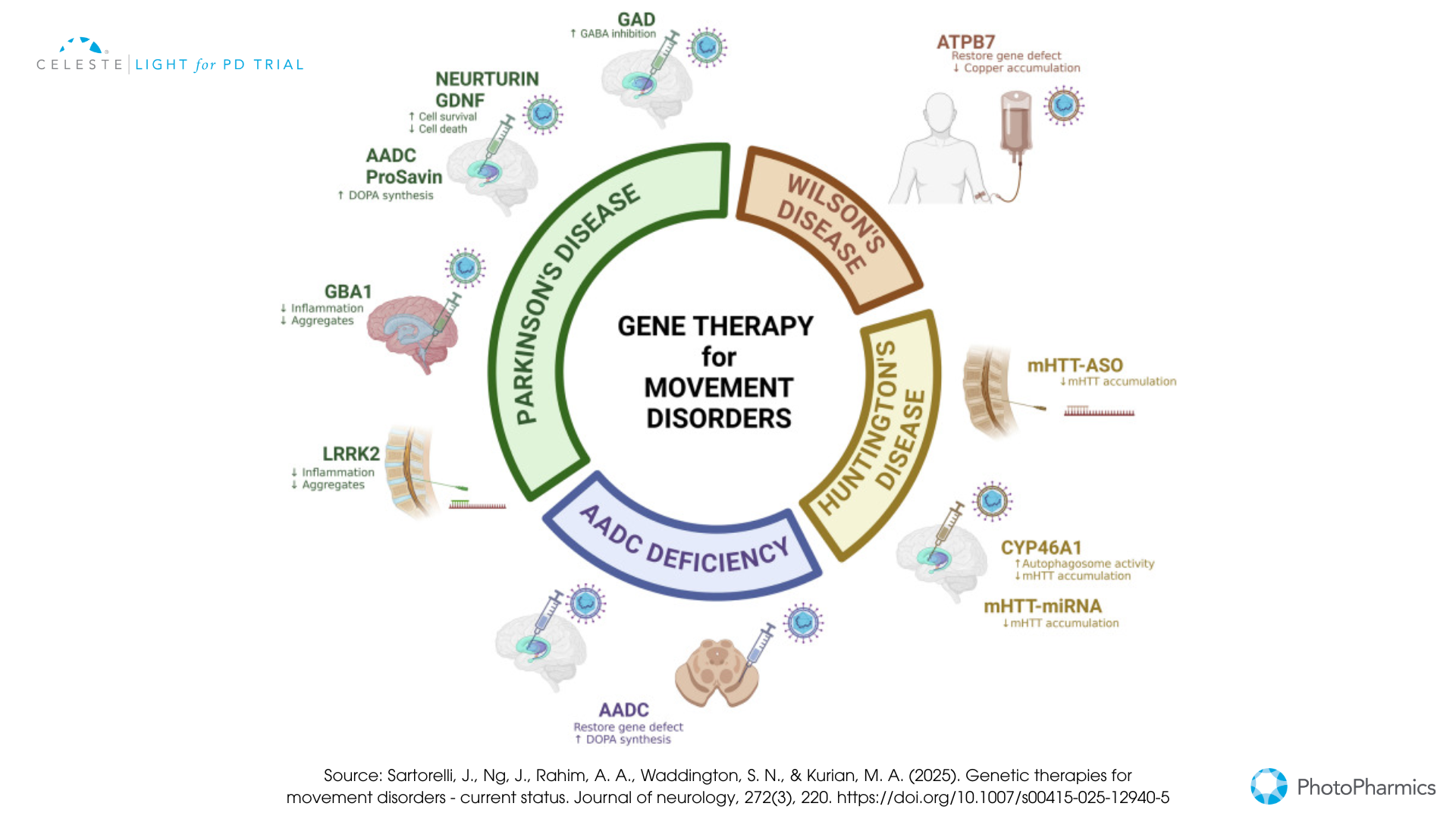
Biological Game-Changers: Gene and Stem Cell Therapies For Parkinson’s
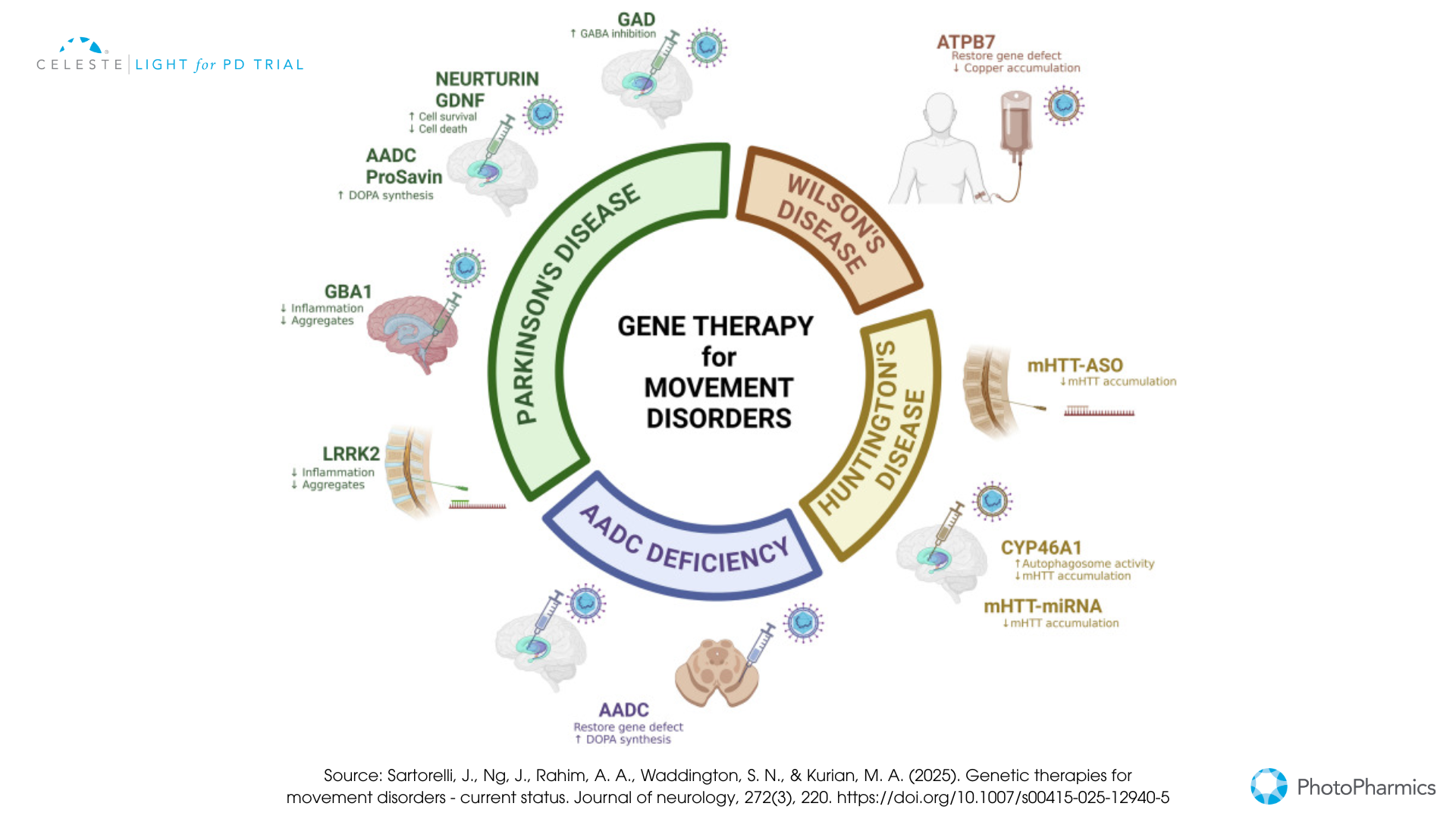
This approach involves delivering genetic material directly into specific brain cells to either restore a lost function, enhance the production of beneficial proteins, or correct a genetic defect.
- Dopamine Replacement Strategies: Some gene therapies aim to help the brain produce more dopamine by delivering genes like AADC (which converts levodopa to dopamine) or a combination of genes needed for dopamine synthesis (e.g., ProSavin, AXO-Lenti-PD).
- Neurotrophic Factors: Others focus on delivering genes that produce protective proteins like GDNF (Glial Cell Line-Derived Neurotrophic Factor), such as AskBio’s AB-1005 (currently in a Phase 2 trial), to shield dopamine neurons from further damage and potentially encourage recovery.
- Targeting Genetic Forms: For Parkinson’s linked to GBA1 mutations, gene therapies like PR001 (in Phase 1/2) aim to deliver a healthy copy of the GBA1 gene. These therapies typically use modified, harmless viruses (like AAV or lentivirus) as delivery vehicles and require neurosurgical procedures.
-
Stem Cell Therapy For Parkinson’s:
The goal here is bold: to replace the dopamine-producing neurons that have been lost.
- How it works: Scientists now take pluripotent stem cells—either human embryonic stem cells, hESCs, or induced pluripotent stem cells, iPSCs, derived from a patient’s own skin or blood. In the lab, they coax these cells to become young dopamine neurons. These new neurons are then surgically transplanted into the brain, usually the putamen.
- Current Status: Several teams worldwide are conducting early-phase clinical trials.
- BlueRock Therapeutics’ bemdaneprocel, derived from hESCs, has shown promising safety and initial efficacy signals in its Phase 1 trial, with some patients experiencing notable motor improvements and evidence of the transplanted cells surviving and functioning. A larger Phase 3 trial is anticipated.
- Aspen Neuroscience’s ANPD001 and a trial at McLean Hospital/Mass General Brigham are pioneering the use of autologous iPSCs (using the patient’s own cells), which avoids the need for immunosuppression. Early results from Aspen’s trial have also been positive regarding safety and initial motor benefits. While incredibly promising, stem cell therapy is still in its early days. Long-term efficacy, the ideal cell type and dosage, and managing potential side effects like graft-induced dyskinesia are key areas of ongoing research.
The progress in these pharmacological and biological frontiers is rapid, bringing the possibility of treatments that not only manage symptoms but also fundamentally alter the course of Parkinson’s disease closer than ever before.
Technology Leading the Way: DBS, Wearables, and AI in Parkinson’s
Technological advancements are profoundly reshaping how Parkinson’s disease is understood, managed, and treated, offering more personalized and precise interventions.
Innovations in Deep Brain Stimulation (DBS)
DBS has been a valuable treatment for advanced Parkinson’s for years, but it’s continuously improving.
- Adaptive DBS (aDBS) or Closed-Loop DBS: This is a major leap forward. Systems like Medtronic’s Percept™ PC with BrainSense™ technology, which recently received FDA approval, can sense and record brain signals (Local Field Potentials, or LFPs, particularly beta-band activity associated with Parkinson’s symptoms). The device then automatically adjusts the stimulation in real-time. This personalized approach aims to deliver optimal symptom control only when needed, potentially reducing side effects like speech issues or dyskinesia, and extending battery life. The ADAPT-PD trial supported its approval, demonstrating its safety and effectiveness.
- Enhanced Precision: Directional leads allow clinicians to “steer” the electrical current more precisely to the target area, avoiding stimulation of nearby structures that could cause side effects. Image-guided programming (IGP), using patient-specific MRI scans and models of the volume of tissue activated, helps clinicians optimize stimulation settings more efficiently, often leading to better outcomes, especially for those who had a suboptimal response to initial programming. Remote programming capabilities are also becoming more common, allowing for adjustments via telehealth and improving access to care.
Wearable Devices in Parkinson’s: Beyond the Clinic Walls
Wearable technology is empowering both patients and clinicians with continuous, real-world data.
- Symptom Monitoring: Small sensors (accelerometers, gyroscopes) worn on the body can track motor symptoms like tremor, bradykinesia (slowness), dyskinesia, and gait disturbances throughout the day. This objective data can help in fine-tuning medication timing and DBS settings, providing a clearer picture of how symptoms fluctuate.
- Drug Delivery: Innovation isn’t just in monitoring. In February 2025, the FDA approved “Onapgo,“ a wearable device that continuously delivers the drug apomorphine hydrochloride subcutaneously. This offers a new way to manage “off” episodes in advanced Parkinson’s, providing more consistent symptom control.
Artificial Intelligence (AI): The Smart Partner in Parkinson’s Care
AI is rapidly becoming an indispensable tool in nearly every aspect of Parkinson’s research and treatment.
- Earlier and More Accurate Diagnosis: AI algorithms are being trained to detect subtle, early signs of Parkinson’s that might be missed by human observation. This includes analyzing voice patterns (changes in pitch, clarity, or speed), subtle shifts in gait captured by sensors or even video, and even changes in handwriting or typing patterns. The goal is to identify the disease at its earliest stages when interventions might be most effective.
- Personalizing Treatment Strategies: As seen with aDBS, AI can interpret complex biological data to tailor treatments. It can also help predict which patients might respond best to certain medications or interventions and assist in optimizing drug dosages or rehabilitation plans.
- Accelerating Drug Discovery and Research: AI can sift through vast amounts of genetic, molecular, and clinical trial data to identify new potential drug targets, repurpose existing drugs for Parkinson’s, or design more efficient clinical trials. Initiatives like Grifols’ Chronos-PD are using AI to analyze plasma samples to find biomarkers that could predict Parkinson’s before symptoms even appear.
These technological tools are not just futuristic concepts; they are increasingly being integrated into clinical practice and research, heralding an era of more precise, data-driven, and patient-centered Parkinson’s care.
Navigating the Path Forward with Hope
The journey with Parkinson’s disease is undoubtedly challenging, but as we’ve explored, the horizon is bright with innovation. From the gentle promise of light therapy and the precision of focused ultrasound to the transformative potential of gene and stem cell therapies, and the smart assistance of AI and advanced DBS, researchers are leaving no stone unturned.
These advancements represent more than just scientific curiosity; they are fueled by a collective global effort to improve the lives of those affected by Parkinson’s and their families.
While many of these treatments are still in various stages of research and development, the pace of discovery is accelerating.
It’s crucial for patients and caregivers to stay informed and maintain an open dialogue with their healthcare team about new and emerging treatment options that might be relevant.
Participating in clinical trials, when appropriate, is also a vital way to contribute to this progress. The path to conquering Parkinson’s is a marathon, not a sprint, but with each new discovery and every dedicated researcher, clinician, patient, and caregiver, we move closer to a future where this disease no longer dictates the terms.
Hope is not just a sentiment; in the world of Parkinson’s research, it is an active, driving force.

Be Part of the Future of Parkinson’s Care with Celeste™
The future of non-invasive Parkinson’s therapy is here — and you could be part of it.
PhotoPharmics’ Light for PD™ trial is currently evaluating Celeste™, a breakthrough light therapy device designed to improve non-motor symptoms of Parkinson’s disease, such as poor sleep, fatigue, mood, and cognitive challenges.
What makes it different?
— It’s non-invasive and used from the comfort of home
— Designed specifically for people with Parkinson’s
— Part of a fully remote clinical trial, open to eligible participants across the U.S.

If you or a loved one is living with Parkinson’s and is interested in advancing treatment options that go beyond medication, we invite you to learn more about the Light for PD™ trial.
Visit lightforpd.com to check your eligibility and see how you can join the trial.
Help us move closer to better, more holistic care for Parkinson’s.
Innovations in Parkinson’s Treatment: Exploring Light Therapy and Beyond
Living with Parkinson’s disease presents daily challenges, not just for those diagnosed but also for their families and caregivers.
It’s a journey that requires resilience, adaptation, and a strong support system. While a cure remains the ultimate goal, the landscape of Parkinson’s treatment is far from static.
Dedicated researchers around the world are tirelessly working on innovative therapies. These efforts offer new hope for managing symptoms and potentially slowing disease progression.
This isn’t just about refining old methods; it signifies a shift towards exploring entirely new avenues. These avenues range from harnessing the power of light to pioneering biological interventions and leveraging cutting-edge technology.
This blog post will take you through some of the most exciting advancements on the horizon. It offers a glimpse into a future where managing Parkinson’s could look very different.
Remember, the field is dynamic, and while some of these innovations are still investigational, they represent the leading edge of scientific discovery aimed at improving lives.

A New Spectrum of Hope: Regulating the Body’s Clock
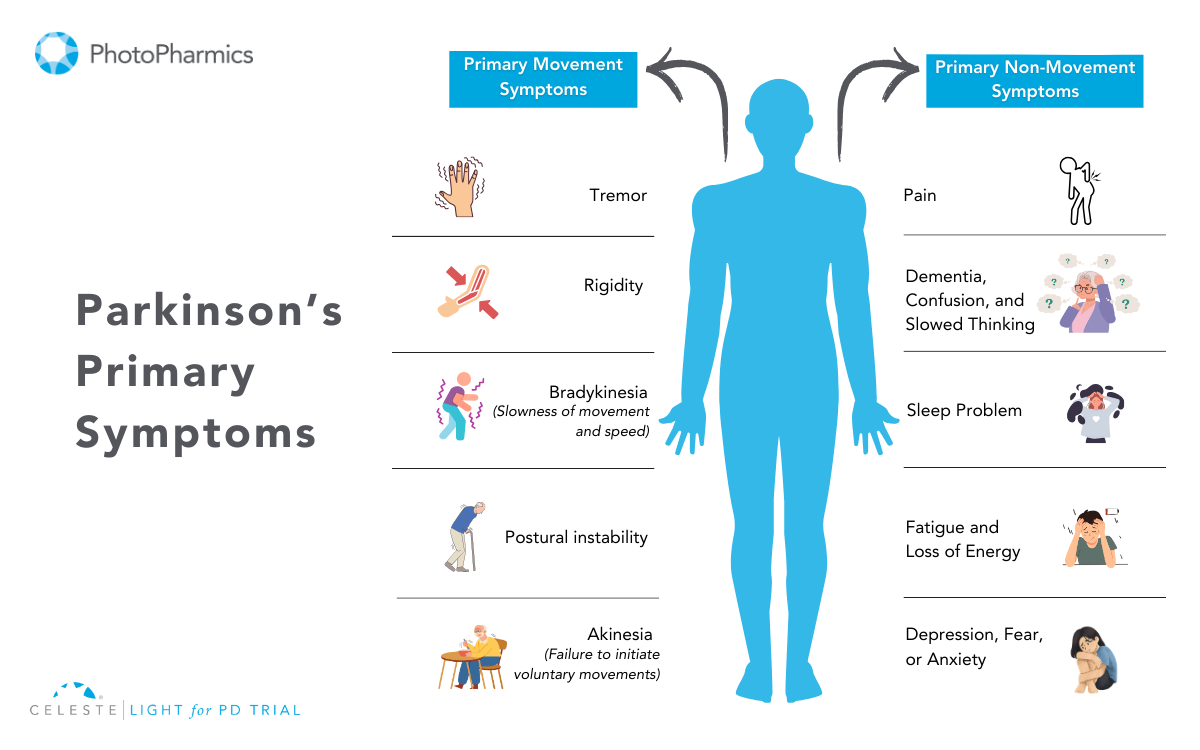
While motor symptoms are the most visible signs of Parkinson’s, the non-motor symptoms—such as poor sleep, depression, and debilitating fatigue—can be just as, if not more, impactful on daily life.
A groundbreaking area of research is now targeting the root cause of many of these issues: a disrupted internal body clock, or circadian rhythm.
This innovative approach moves away from pharmacological solutions. It asks a different question: what if we could use light itself to help restore the body’s natural balance?
This therapy, pioneered by PhotoPharmics, explores a powerful idea: light influences brain activity. Specifically, it focuses on the profound connection between light, the brain, and our daily rhythms.
Introducing The Celeste® device
In a healthy individual, the body’s master clock is located in a brain region called the suprachiasmatic nucleus (SCN). It is synchronized by light signals received through the eyes. This light-regulated process influences our sleep-wake cycle, mood, and energy levels. Unfortunately, dopamine loss in Parkinson’s disrupts this system and triggers many non-motor symptoms.
The therapeutic solution is a specialized, non-invasive phototherapy device, such as the Celeste® device. It works by delivering specific, spectrally-opposed wavelengths of light to the user at programmed times of the day.
This light is not ordinary; it’s highly calibrated. It targets specific retinal cells that signal the brain’s master clock. The goal is to gently and effectively regulate and reset the user’s circadian rhythm without drugs.
By restoring a more normal day/night cycle, this therapy aims to produce a domino effect of positive benefits. A well-regulated circadian rhythm can lead to improved sleep consolidation and quality.
In turn, better sleep is foundational to improving mood, reducing the burden of depression, increasing daytime energy, and sharpening cognitive function. This approach tackles the underlying dysfunction rather than just masking the individual symptoms.
This therapy is the subject of the “Celeste Light for PD Trial,” a large Phase 3 study evaluating its effectiveness in Parkinson’s. Unlike many investigational treatments, this therapy is designed to be used at home, integrating seamlessly into a person’s daily routine.
Generally, this form of phototherapy is considered very safe. It represents a beacon of hope for managing the challenging non-motor symptoms of Parkinson’s, offering a non-pharmacological approach that could complement existing treatments.
However, more large-scale, rigorously controlled clinical trials like the Light for PD study are essential to confirm its efficacy before it can become a mainstream option.
Non-Pharmacological Parkinson’s Treatment Strategies
While light therapy charts a novel path, other non-drug treatments are also evolving, offering new ways to manage Parkinson’s symptoms.
Focused Ultrasound: A Novel Parkinson’s Treatment Approach
Imagine a surgical outcome without the scalpel. That’s the promise of MR-guided Focused Ultrasound. This FDA-approved technology uses intersecting ultrasound beams, guided by real-time MRI. It precisely heats and destroys a small target area in the brain, causing motor symptoms.
For Parkinson’s, FUS can target the Ventral Intermediate Nucleus (VIM) of the thalamus, primarily to alleviate medication-refractory tremor, or the Globus Pallidus Interna (GPi) to address other motor issues like stiffness, slowness, and dyskinesia. The major advantage is that it’s incisionless, offering immediate symptom relief for many.
However, the lesion created by Focused Ultrasound is permanent. For this reason, the procedure is typically done on only one side of the brain to minimize risks like speech or swallowing issues.
Research is ongoing to refine this technology and explore its potential for temporarily opening the blood-brain barrier to facilitate drug delivery.
Transcranial Magnetic Stimulation (TMS)
TMS is another non-invasive technique that uses magnetic pulses to gently modulate the activity of specific brain regions. Depending on the frequency and pattern of the pulses, TMS can either excite or inhibit neuronal activity. For Parkinson’s, it’s being investigated for various motor symptoms, particularly for improving gait and reducing Freezing of Gait (FOG).
Non-motor symptoms like depression (for which it has FDA approval) and cognitive issues are also being targeted. Some deep TMS systems have gained regulatory approval outside the US for Parkinson’s motor symptoms.
While generally safe, the benefits of TMS can sometimes be temporary, and researchers are working to optimize treatment protocols for longer-lasting effects.

Novel Rehabilitation Strategies
Rehabilitation remains a cornerstone of Parkinson’s care, and it too is undergoing an innovation wave. There’s a growing emphasis on holistic, personalized programs that integrate traditional therapies with new technologies.
-
Virtual and Augmented Reality (VR/AR) systems are changing how people with Parkinson’s approach exercise. They create engaging, game-like environments to make movement fun. These tools help improve motor control, balance, and even cognitive engagement during physical activity.
- Robotics are being used to provide intensive, repetitive training for gait and upper limb function, offering consistent and quantifiable therapy.
- Specialized exercise programs like LSVT BIG® (for movement amplitude) and LSVT LOUD® (for voice power) continue to show strong evidence for improving motor and speech functions.
- Dual-task training, which involves performing a cognitive task while executing a motor task, is gaining traction to address the difficulties many people with Parkinson’s experience with divided attention.
- Mind-body interventions like Tai Chi, yoga, and mindfulness meditation are also being recognized for their benefits in improving balance, flexibility, mood, and overall quality of life.
These innovative non-pharmacological approaches offer valuable alternatives and adjuncts to medication, empowering individuals to take an active role in managing their condition.
Advancements in Drug-Based Parkinson’s Treatment
The search for better medications and biological therapies is at the heart of Parkinson’s research, with a significant shift towards treatments that could potentially slow or even halt disease progression, rather than just managing symptoms.
Targeting the Core Pathology: New Drug Candidates
-
- This protein, which misfolds and clumps together to form Lewy bodies, is a hallmark of Parkinson’s. Many new drugs aim to tackle it directly.
- Immunotherapies: This approach involves several strategies. Vaccines aim to train the immune system. They help it recognize abnormal alpha-synuclein. The goal is to clear this protein. An example is UB-312. It showed target engagement in early trials. Monoclonal antibodies are another method. These are directly administered. They bind to the problematic protein. This helps remove alpha-synuclein. Prasinezumab is one example. It has shown some positive signals in Phase 2 trials.
-
Neuroinflammation and Mitochondrial Health:
- Chronic inflammation in the brain and dysfunction in the mitochondria (the cell’s energy factories) are recognized as key contributors to Parkinson’s progression.
- Drugs targeting the NLRP3 inflammasome (an inflammatory complex), such as Dapansutrile (currently in Phase 2), aim to quell this damaging inflammation.
- c-ABL inhibitors, like Risvodetinib and Vodobatinib (both in Phase 2 trials and showing good brain penetration), are being investigated for their potential to protect neurons by reducing oxidative stress and improving the clearance of alpha-synuclein.
-
Genetic Clues Paving New Paths:
- For individuals with specific genetic links to Parkinson’s, more personalized treatments are emerging.
- GBA1 Gene Mutations: These are a significant risk factor. Therapies aim to boost the activity of the GCase enzyme, which is deficient in these individuals. Ambroxol (a repurposed cough medicine) is in a large Phase 3 trial (ASPro-PD), and BIA 28-6156 is a GCase activator currently in Phase 2.
- LRRK2 Gene Mutations: Several companies are developing LRRK2 kinase inhibitors, with some candidates now in clinical trials.

-
Repurposed and Novel Mechanisms:
Looking Ahead: Part 2 and a Vital Clinical Trial Opportunity
In Part 2 of “Innovations in Parkinson’s Treatment,” we will delve into the exciting realms of gene and stem cell therapies – biological game-changers that aim to restore lost function or protect remaining neurons.
We’ll also explore how cutting-edge technology, including advanced Deep Brain Stimulation (DBS), wearable devices, and the transformative power of Artificial Intelligence (AI), is reshaping how Parkinson’s is understood, managed, and treated.
Want to be part of pioneering research for Parkinson’s non-motor symptoms?
The “Light for PD” clinical trial, testing the Celeste phototherapy device, is making significant strides with over 200 patients already enrolled! This crucial study is nearing its final stages. If you or a loved one with PD is interested in exploring this non-invasive approach to manage non-motor symptoms like poor sleep, depression, and fatigue, now is the critical time to act.
Don’t miss your chance to contribute.
Learn more and inquire about joining the Light for PD trial before enrollment closes: https://www.lightforpd.com/
Introduction
Parkinson’s is one of the most common neurodegenerative disorders, second only to Alzheimer’s. Globally, it affects around 1% of people over 60, making it the leading movement-related neurological condition.
“Parkinson’s diagnosis and treatment options” is one of the most common concerns for individuals living with Parkinson’s and their families. The uncertainty surrounding symptoms, medical evaluations, and treatment plans can feel overwhelming.
That’s why we’ve created this guide—to answer your most pressing questions and help you navigate the path forward with clarity and confidence.
Parkinson’s disease is a progressive neurological condition that affects movement, coordination, and other vital functions. Because symptoms often develop gradually, diagnosing Parkinson’s can be complex, requiring a detailed medical history, neurological exams, and, in some cases, advanced imaging tests.
While there is no single definitive test, early and accurate diagnosis is key to managing the condition effectively.
Once diagnosed, treatment options vary depending on the stage of the disease and individual needs.
From medications that help manage symptoms to therapies like physical and occupational therapy, each approach aims to enhance quality of life. In more advanced cases, surgical interventions such as deep brain stimulation (DBS) may offer relief. Additionally, emerging treatments and clinical trials provide hope for future breakthroughs.
While Parkinson’s presents challenges, proactive management, and the right treatment plan can make a significant difference. I
In this article, we’ll explore the available diagnostic tools, current treatments, and promising advancements in Parkinson’s care, helping you or your loved one take informed steps toward better health and well-being.

1. Understanding Parkinson’s Disease
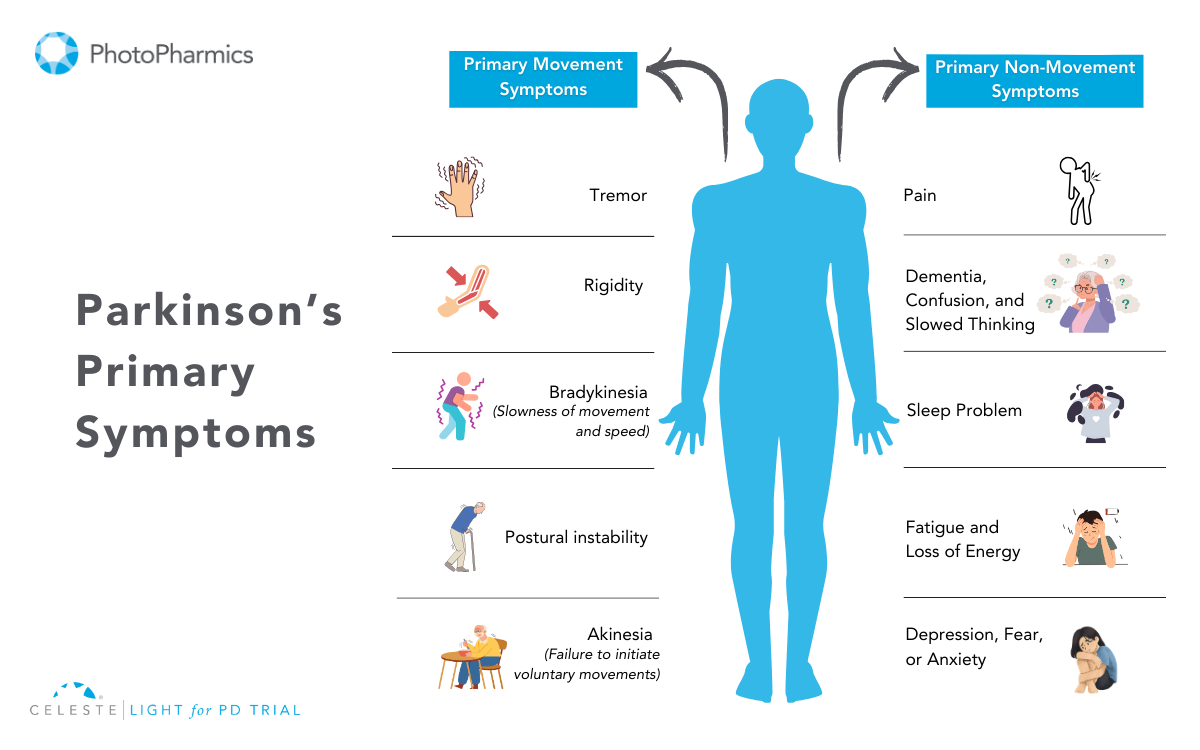
Parkinson’s disease is a disorder that gradually affects the brain’s ability to control movement. It occurs due to the deterioration of nerve cells in a region called the basal ganglia, which leads to a decline in dopamine production. Dopamine is essential for smooth and coordinated muscle activity, and its deficiency causes symptoms like tremors, muscle stiffness, and slowed movement.
However, Parkinson’s isn’t just a movement disorder. As it progresses, it can affect various aspects of life, including cognition, mood, sleep, and sensory functions. Many individuals experience depression, memory challenges, and difficulties with speech or swallowing. Though no cure exists, early diagnosis and proper management can significantly improve daily functioning.
Who is at Risk?
Parkinson’s is primarily an age-related condition, with most cases diagnosed around 60 years old or older. The risk increases with age, but it is not limited to the elderly. A small percentage of cases, known as early-onset Parkinson’s, occur in younger adults, sometimes as early as their 20s or 30s. These cases are often linked to genetic factors, meaning a close relative may also have had the disease.
Men are slightly more likely than women to develop Parkinson’s, but the reason behind this difference remains unclear. Scientists continue to study genetic and environmental factors that may contribute to disease onset.
Parkinson’s and Related Conditions
The term “parkinsonism” is a broader term that includes Parkinson’s disease and other conditions that have similar symptoms. These other conditions might include multiple system atrophy or corticobasal degeneration.
Parkinson’s disease, specifically, is characterized by the degeneration or impairment of the neurons in the basal ganglia that produce dopamine. It’s this dopamine deficiency that directly causes movement-related problems. The actual cause of the damage to these neurons is not yet fully understood.
Parkinson’s is a brain disorder that results in unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination. 1 Symptoms usually begin gradually and worsen over time.
As the disease progresses, individuals might experience difficulty walking and talking. Mental and behavioral changes, sleep problems, depression, memory issues, and fatigue can also occur.
While anyone can be at risk for developing Parkinson’s, research suggests that it affects more men than women. The reasons for this are not yet clear, but research is being conducted to identify factors that might increase a person’s risk.
Age is a known risk factor: Although most people with Parkinson’s are diagnosed after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinson’s are sometimes, but not always, inherited, and some forms have been linked to specific genetic changes.
Understanding Parkinson’s Disease: Diagnosis and Treatment
Parkinson’s disease (PD) is a progressive neurological condition that affects movement and various other bodily functions. While there is currently no cure, early diagnosis, and effective treatment can significantly improve the quality of life for those living with the disease.
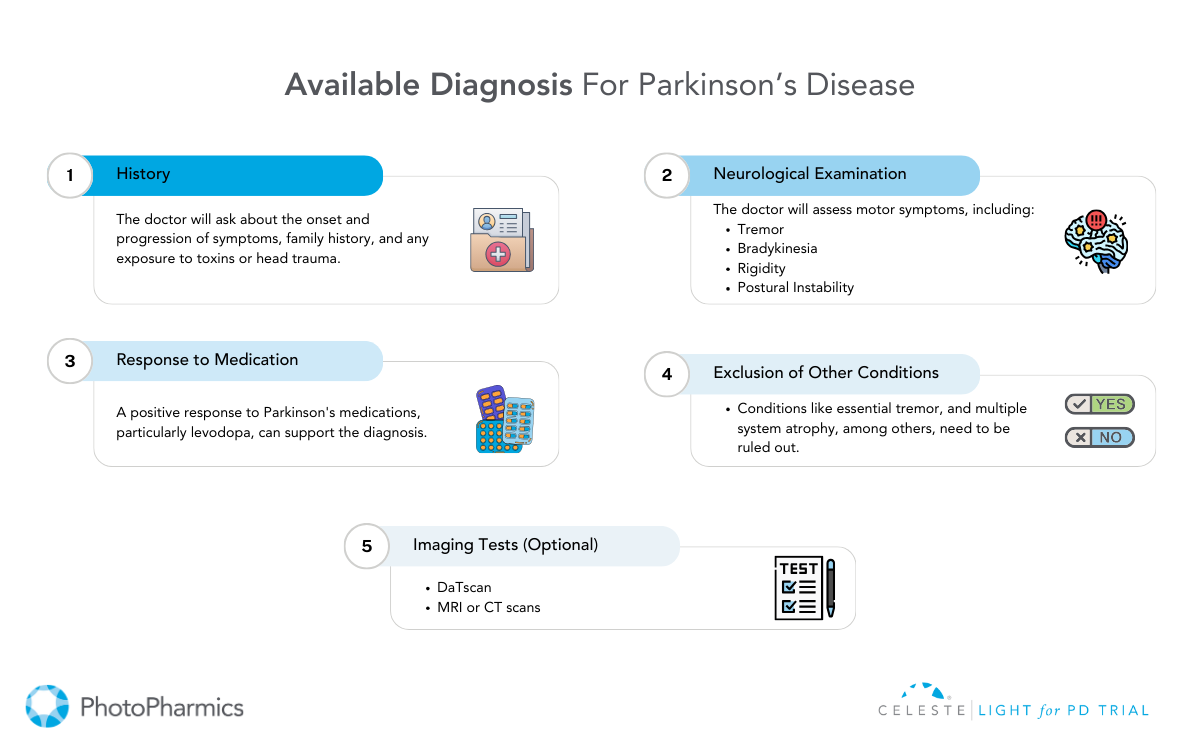
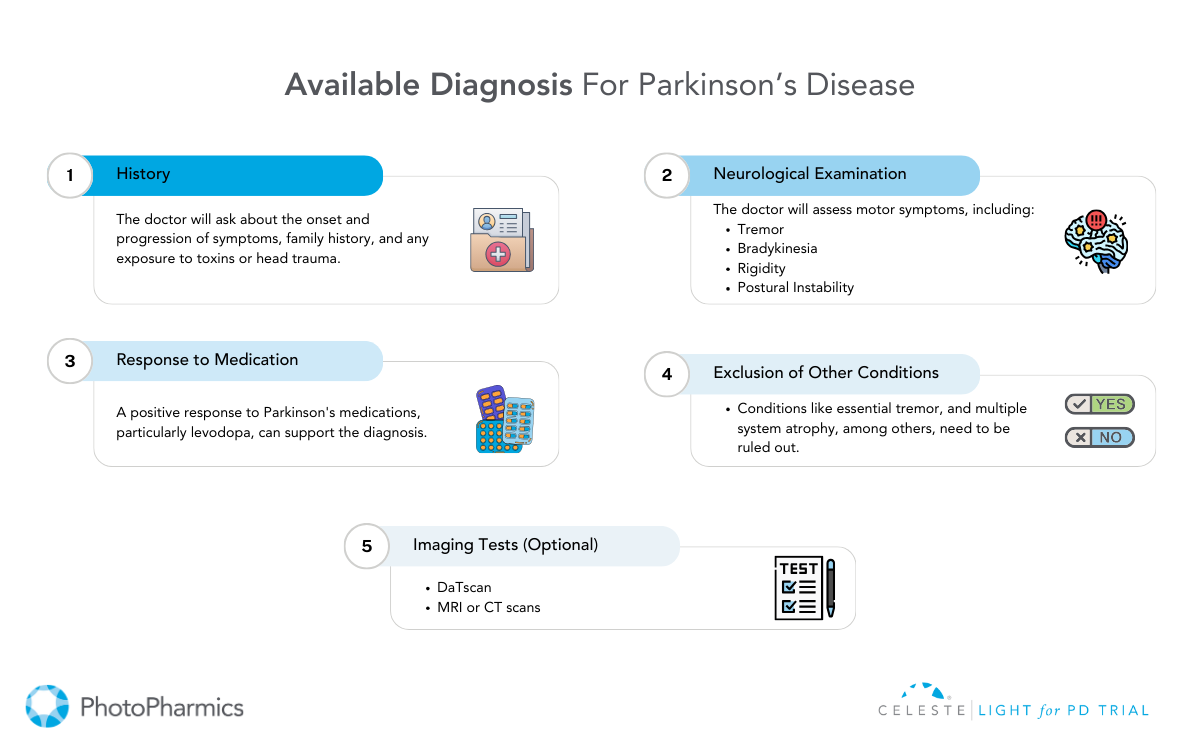
Diagnosing Parkinson’s Disease
Diagnosing Parkinson’s disease is primarily a clinical process. There is no single test that can confirm the condition. Instead, healthcare providers rely on a combination of medical history, symptom evaluation, and physical examinations. Laboratory and imaging tests are sometimes used to rule out other conditions that mimic Parkinson’s.
Common Diagnostic Approaches
- Medical History & Symptom Assessment: Doctors evaluate symptoms such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability.
- Neurological Examination: A detailed physical examination helps assess muscle stiffness, reflexes, coordination, and movement issues.
- Levodopa Response Test: If a patient’s symptoms improve with levodopa medication, it often confirms Parkinson’s.
Imaging and Laboratory Tests
While imaging and lab tests cannot diagnose Parkinson’s definitively, they help rule out other conditions. These include:
- Blood Tests: While not diagnostic for Parkinson’s, blood tests can help exclude other medical conditions that might be contributing to or mimicking the symptoms, such as thyroid problems or vitamin deficiencies.
- MRI & CT Scans: A CT scan uses X-rays to create cross-sectional images of the brain. It’s primarily used to visualize brain structures and rule out structural abnormalities like tumors or strokes that could be causing the symptoms.
- An MRI scan uses magnetic fields and radio waves to create detailed images of the brain. Like CT scans, MRIs help visualize brain structures and rule out other causes of symptoms. They can also sometimes help differentiate Parkinson’s from other neurodegenerative conditions.
- PET Scans: A PET scan uses a radioactive tracer to visualize brain activity. While not routinely used for Parkinson’s diagnosis, PET scans can sometimes help differentiate Parkinson’s from other conditions by showing patterns of brain activity. For example, a DaTscan, a type of PET scan, can visualize dopamine transporters in the brain and help confirm a diagnosis of Parkinsonian syndrome.
- Genetic Testing: Genetic testing may be considered in specific circumstances, such as early-onset Parkinson’s (diagnosed before age 50) or a strong family history of the disease. Certain genetic mutations are associated with an increased risk of Parkinson’s, though most cases are not directly linked to specific genes.
New Advances in Diagnostic Testing
- Spinal Tap (Lumbar Puncture): Researchers have found that analyzing cerebrospinal fluid for misfolded alpha-synuclein proteins may help in diagnosis.
- Skin Biopsy: A small sample of skin tissue is tested for abnormal alpha-synuclein deposits, which could indicate Parkinson’s disease.
Treatment and Management of Parkinson’s Disease
While Parkinson’s is incurable, various treatment strategies can help manage symptoms and enhance quality of life. Treatment plans are typically personalized based on symptom severity, progression, and individual response to therapy.
Medications for Parkinson’s Disease
Medications are the primary treatment for managing Parkinson’s symptoms. These fall into two main categories:
- Dopamine Replacement & Enhancement
- Levodopa: Levodopa is a precursor to dopamine and is converted into dopamine in the brain. It’s the most effective medication for managing motor symptoms, particularly bradykinesia and rigidity. However, long-term use can lead to motor fluctuations (on-off periods) and dyskinesia (involuntary movements).
- Levodopa-Carbidopa Combination: Carbidopa prevents levodopa from breaking down before reaching the brain, reducing side effects.
- Levodopa Metabolism Inhibitors: These medications, such as entacapone and tolcapone, prolong the effects of levodopa by inhibiting the enzyme COMT, which breaks down levodopa. They are typically used in combination with levodopa to manage motor fluctuations.
- Dopamine Agonists
- These medications mimic the action of dopamine in the brain, stimulating dopamine receptors. They can be used alone in early-stage Parkinson’s or in combination with levodopa. Common side effects include nausea, dizziness, sleepiness, and, in some cases, impulse control disorders.
- Other Medications
- Dopamine Metabolism Blockers: Help preserve dopamine levels in the brain.
- Adenosine Blockers: These medications, such as istradefylline, work on a different neurotransmitter system and can be used as an add-on therapy to levodopa to improve motor function.
- Amantadine: Helps reduce involuntary movements (dyskinesia).
- Anticholinergic Drugs: Assist in reducing tremors and muscle rigidity.
- MAO-B Inhibitors: These drugs block the enzyme monoamine oxidase B, which breaks down dopamine. By inhibiting this enzyme, MAO-B inhibitors help increase dopamine levels in the brain. They are often used in early-stage Parkinson’s or as an adjunct to levodopa.
Surgical Treatment: Deep Brain Stimulation (DBS)
For patients whose symptoms do not respond well to medication, Deep Brain Stimulation (DBS) is a surgical option.
- How it Works: Electrodes are implanted in specific brain areas and connected to a small device placed in the chest, which sends electrical impulses to regulate abnormal brain activity.
- Benefits: Reduces tremors, rigidity, and motor fluctuations, offering greater movement control.

Experimental Treatments & Future Research
Researchers are continuously exploring innovative treatments:
- Stem Cell Therapy: Aims to replace damaged neurons with healthy dopamine-producing cells.
- Neuron Repair Treatments: Focuses on regenerating and protecting nerve cells.
- Gene Therapy: Targets specific genetic mutations to slow disease progression.
- Light Therapy: Emerging research suggests that light therapy may help regulate circadian rhythms, improve sleep, and reduce non-motor symptoms in Parkinson’s patients.
Light for PD, a clinical trial by PhotoPharmics, explores how specialized light therapy can enhance the quality of life for individuals with PD.
Supportive Therapies and Lifestyle Management
Comprehensive care extends beyond medication and surgery. Supportive therapies can help patients maintain mobility, independence, and overall well-being.
- Physical Therapy: Enhances movement, flexibility, and strength.
- Occupational Therapy: Assists in daily activities and adaptive techniques.
- Speech Therapy: Helps with communication and swallowing difficulties.
- Dietary Changes: A balanced diet rich in fiber, antioxidants, and hydration supports overall health.
- Exercise & Alternative Therapies: Activities like yoga, tai chi, and massage therapy improve balance and flexibility.
If you or a loved one is affected by Parkinson’s, consult with a healthcare professional to explore the best treatment options
On Stable Meds But Still Not Satisfied?
Research continues to explore new therapies, including gene therapy, neuroprotective drugs, and innovative treatments like light therapy.
A promising investigational FDA Breakthrough device, “Celeste,” is in the clinical trials, being developed to improve both motor and non-motor symptoms in Parkinson’s disease. This at-home light therapy device aims to enhance quality of life beyond current medications.

Why Join the Trial?
- No travel or medication changes are required.
- Open to anyone with Parkinson’s in the U.S.
- Convenient, and used during daily activities.
- No cost to participants—they receive $500 for completing the trial.
Is There a Better Way to Manage PD Symptoms?
Many people with PD experience lingering symptoms like fatigue, sleep issues, and anxiety.
Celeste offers a non-drug alternative designed to address these unmet needs. Learn more and see if you qualify for the Celeste Light for PD Trial today!